There is a growing body of evidence on the effect of behavioral health and cognitive disorders on physical health. Dr. Helen Ouyang, an emergency room physician, in a recent guest essay in The New York Times, opined, “We need a care system and medical culture that support the health of the whole person. My patients already seem to grasp this truth. Many of them are eager for integrated care that prevents both mental and physical illness. Now the health care system needs to catch up to their wisdom so that we can help them do so.”
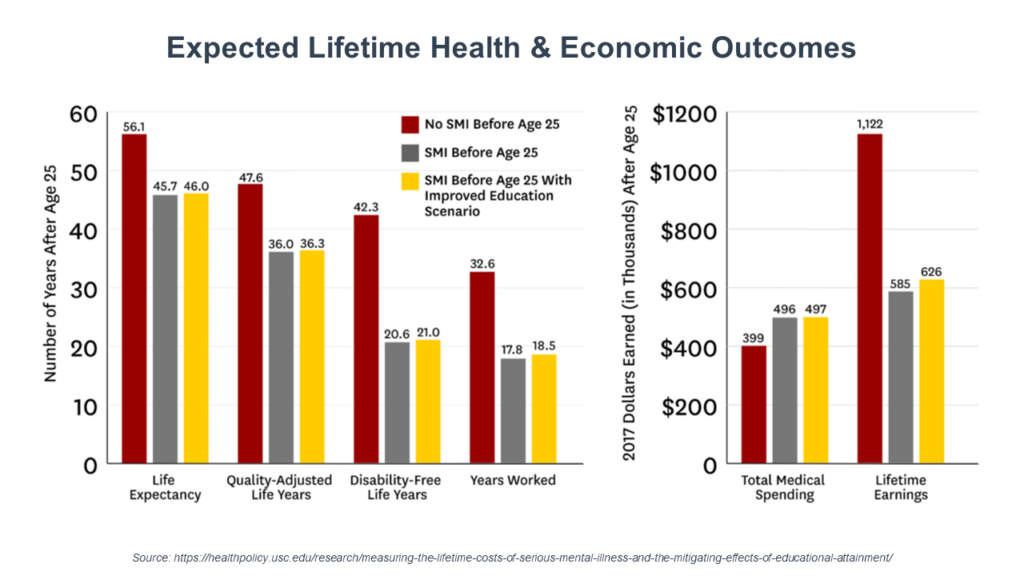
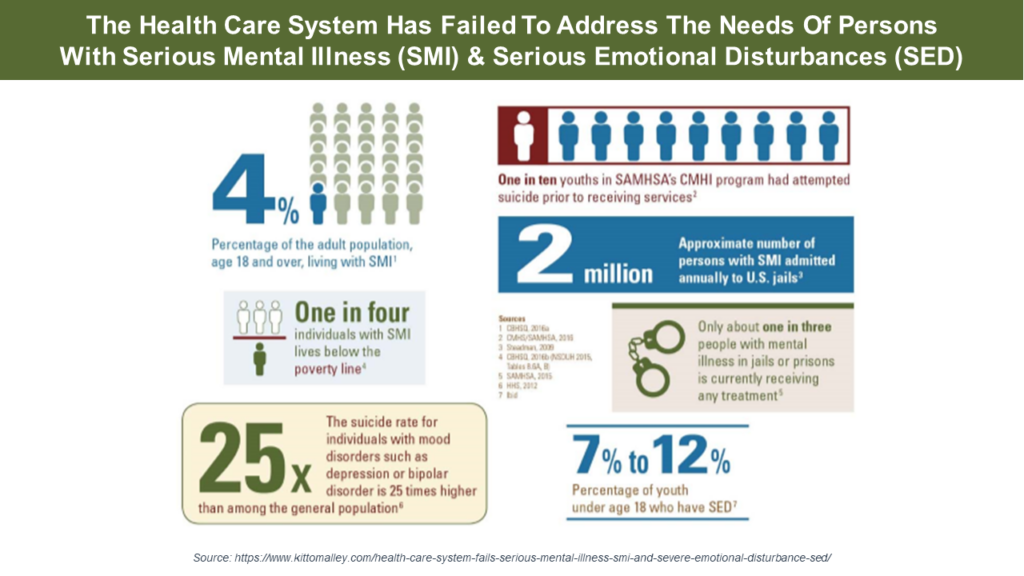
The most simplistic measure of this relationship is life span. A 2023 meta-analysis found that people with substance use disorder (SUD) had a life expectancy of 57 years, with a serious mental illness (SMI), 64 years, and with neurotic disorders, 69 years–compared to the Center For Disease Control’s estimate of an average life span of 77.5 years for those without mental health issues. Of interest to payers, consumers with chronic medical conditions who received mental health services saw a 22% reduction in their total health care expenses.
Movement toward whole person care models and integrated delivery systems continues across the health and human service field, but integrated approaches to consumer care are still the exception rather than the rule—and fragmentation of funding and services is still common. What are the approaches being used to move the system in that direction?
We got a preview of several new initiatives integrating services coordination and service delivery at the consumer level during a recent discussion with James Polo, M.D., Chief Medical Officer of Carelon Behavioral Health. Carelon is using both projective analytic tools and field-based initiatives to “bridge the gaps” for consumers and provide a holistic approach to their care.
Carelon has prioritized prevention and intervention using projective analytic tools. “It’s a way of using our data and using our analytic abilities to actually get ahead of the problem rather than behind it,” Dr. Polo explained. One such tool with which Carelon has had success is a suicide prevention application. “Lots of crisis activities are going on just because of a limited workforce and huge demand for services,” he said. “And helping get the actual care that they need is challenging in the crisis arena. In the last two to three years, we’ve seen an increase of suicide rates—and the issue is that they aren’t in treatment or they’re having difficulty finding treatment, or the treatment they’re getting is not sufficient for them to have hope.”
“We have a tool targeting individuals aged 5 through adult that uses projective analytics to look at our data so that we can identify by population cohort the individuals that our data tells us are very high likelihood to have a self-harm event in the in the following 12 months. This allows us to focus on those at-risk individuals to help avoid the possibility of an adverse outcome.”
And Dr. Polo said they have the performance metrics that indicate positive results: “Our data demonstrates that we are having tremendous success essentially in lowering rates of self-harm in lowering rates of suicide in in our populations and a variety of different states where we’ve launched.”
Beyond technological tools, Carelon has focused on field-based initiatives like the “Hope” program, a “boots on the ground” effort to uncover employment issues, housing and food insecurity and identify the mental health and substance use challenges to address them in a holistic manner. As Dr. Polo described, “We are connecting consumers with primary care assets to make sure that they’re getting their physical health needs met and making sure that we’re providing behavioral health interventions.”
Carelon has also implemented field-based initiatives in treatment of the serious mental illness (SMI) population—with its outreach to consumers with schizophrenia, schizoaffective disorder, severe bipolar, and major depression. “Again, we deploy field-based programs to engage these individuals face-to-face to look at their behavioral challenges and any the medical problems they’re struggling and connect them to care. These models are live currently in five states in the country and we’re going into three more markets this year. We’re adding even more next year.”
Delivering integrated care is a challenge to both health plans and provider organizations—with issues in technology, reimbursement, and culture making it difficult. Dr. Polo reflected on this in our discussion. “I think what we all struggle is the need to come together and ask, ‘What are the right things that we can incentivize that will be good for all folks, not just one population as a way of making it easy for providers to do what’s right.’”
