By Monica E. Oss, Chief Executive Officer, OPEN MINDS
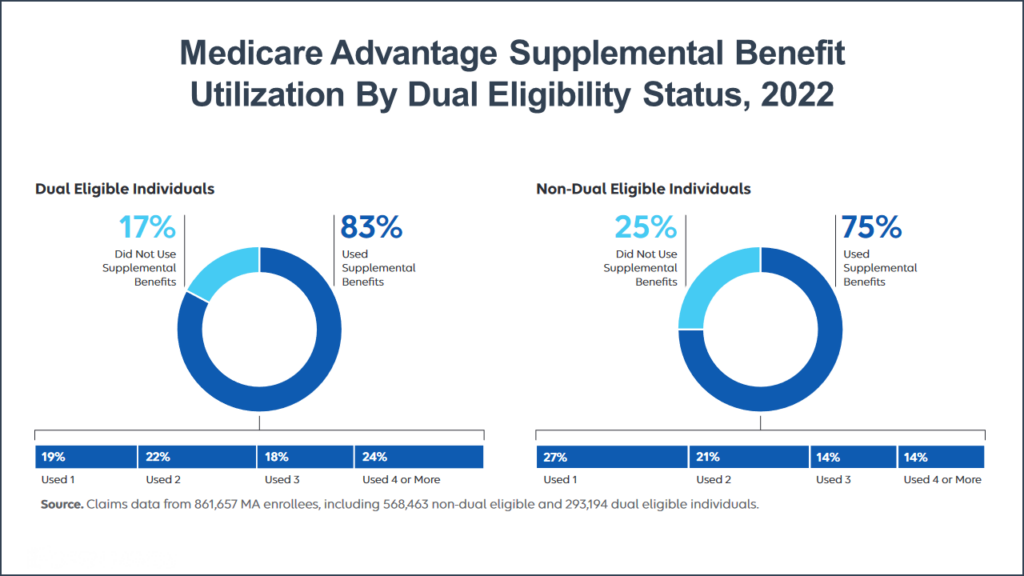
Whole person care is certainly popular with the Medicare population. 83% of dual-eligible and 75% of non-dual-eligible individuals in Medicare Advantage plans used at least one supplemental benefit a year. Those figures only drop to 64% and 48%, respectively, for using at least two different supplemental benefits. These were the findings of recent research by the Elevance Health Public Policy Institute, published in a new report, Medicare Advantage Supplemental Benefits Address Health-Related Social Need.
In 2019, CMS permitted Medicare Advantage plans to offer supplemental benefits beyond vision and dental. benefits and value-added benefits. These additional benefits can include vision or dental coverage, hearing aids, nutrition benefits and medically-tailored meals, transportation services, housing supports, gym and wellness services, and selected use of inpatient behavioral health facilities known as institutions for mental disease (IMDs). But the focus on a whole person care approach to population health is not limited to Medicare. Medicaid health plans are now allowed to spend up to 5% of their medical loss ratio on programs focused on meeting the social support needs of beneficiaries.

For specialty and primary care provider organization executive teams that want to take advantage of this new market niche and develop targeted services for specific consumer populations, what gives provider organizations an ‘edge’ on a preferred relationship with a health plan? That was the question our team posed to Beau Hennemann, Regional Vice President of Local Engagement at Anthem Blue Cross – California Medicaid. His short answer—the ability to deliver services using a whole person approach and plugging into integrated delivery systems. He said, “We are working towards a health care delivery system that is focused on whole person needs, pulling in all the pieces of an individual’s life to build fully integrated systems of care.”
Mr. Hennemann will be expanding on this perspective in his keynote presentation Leveraging Technology To Manage For Quality: How Anthem Blue Cross Is Using Data, Analytics & Metrics To Improve Population Health on October 27th at The 2023 OPEN MINDS Technology & Analytics Institute in Philadelphia. Anthem Blue Cross’ California Medi-Cal plan serves 1.6 million members, members whose needs vary significantly from community to community, according to Mr. Hennemann. To address those needs, several years ago, Anthem started its first pilot programs to use community data to develop custom programs for specific populations. Today, those initial pilots have grown into a data-driven approach to identifying key partners and developing critical interventions. The data allows Anthem to “connect the dots” across multiple lines of services to map out “hot spots” and programs that address critical community needs as diverse as housing, homelessness, food insecurity, and unemployment.
As a result, Anthem has built relationships with more than 150 provider organizations—ranging from large multi-jurisdiction organizations to Federally Qualified Health Centers (FQHC) to small specialty organizations. This has changed what Anthem looks for when partnering with provider organizations. Mr. Hennemann stressed three “key ingredients” that are the top of the Anthem list—strong community presence, a proven track record of service delivery, and a willingness to adopt new clinical and administrative processes—including new reporting requirements.
Strong Community Presence As Anthem Blue Cross is developing solutions in specific communities, its team is looking for provider organizations that are strong players at the local level. Making whole person care work requires organizations that can coordinate all the resources that a community has to build a connected web of care that is supportive, accessible, and comprehensive to whole person needs. Provider organizations need a strategy to become a ‘partner of choice’ in their community.
A Proven Track Record Of Service Delivery These new partnerships present an opportunity to expand service delivery—to new consumers, new geographies, and new services. But to be considered, health plans are looking for a demonstrated successful track record with current services. Executive teams should be prepared to report on the performance and clinical outcomes of their current services. Communicating those results is key to positioning as a reliable partner for the health plan.
Willingness To Adopt New Clinical And Administrative Processes—Including New Reporting Requirements Provider organization executive teams need the ability to change—enhancing current services and developing new services to meet the changing needs of health plan members. Partnerships are a two-way street and “willingness to adapt” is a key ingredient for success, according to Mr. Hennemann. He stresses that provider organization leadership buy-in is a critical component to efficient partnerships.
One of the significant challenges for these emerging partnerships is in data gathering and performance reporting. The ability to report on claims, evaluations, consumer engagement, and care coordination processes are just the start. And reporting specifications can vary from program to program—and change over time.
For many provider organizations, the ability to serve consumers with the most complex needs is a market differentiator. For many, the knowledge of the consumer and the local community are positive differentiators. But the infrastructure to operate high-performing programs—reporting on that performance—is a requirement for future success.
