I was attracted to the headline—Stop Using ‘Whole Person Care’ If You Are Not Assessing And Providing Whole Person Care. In the piece, author Scott Conard, M.D., makes the case that the term “whole person care” (WPC) is becoming a hackneyed slogan.
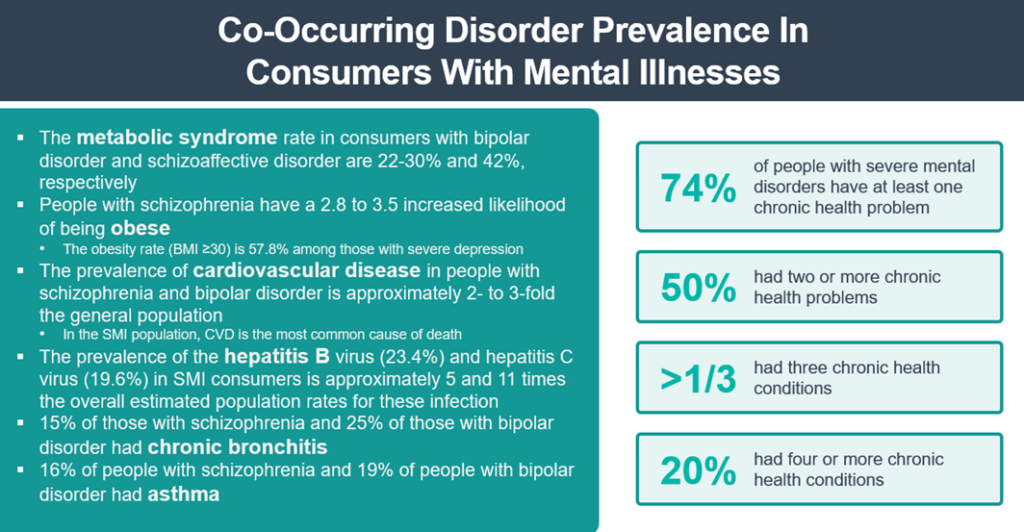
He defines the term as “looking at the whole person—not just separate organs or body systems—and considering multiple factors that promote either health or disease. It means helping and empowering individuals, families, communities, and populations to improve their health in multiple interconnected biological, behavioral, social, and environmental areas. Instead of just treating a specific disease, whole person health focuses on restoring health, promoting resilience, and preventing diseases across a lifespan”. His perspective—“Whole person care must encompass the following essential components: physical, emotional, social (including community), financial, and spiritual well-being.”
Dr. Conrad points out some of the misuses of the term online. In one instance, WPC is defined as integrating physical and mental health care, but “this definition overlooks 60% of the concept and dilutes the true meaning of whole person care.” His perspective—making access to traditional health care easier is not whole person care.
In another, WPC is defined as “…making drugs less expensive, integrating with specialists more effectively for eye and dental care, integrating behavioral health benefits, reducing out-of-pocket expenses… and providing wrap-around wellness programs.” His response—making access to traditional health care easier is not whole person care.
This week, I had the opportunity to address the ACCELERATE Conference sponsored by ContinuumCloud on the state of whole person care and integrated delivery systems in my keynote, “Building A Connected Ecosystem For Better Service Delivery In Behavioral Health: The Whole Person Care Imperative”. The prevalence of integrated delivery systems (defined as a method of structuring services to support the delivery of whole person care which requires collaboration between disciplines, implementing new technologies, and adapting payment models) is on the rise. The challenge is that there are 80+ models of integrated care—a strategic challenge for most provider organization executive teams.
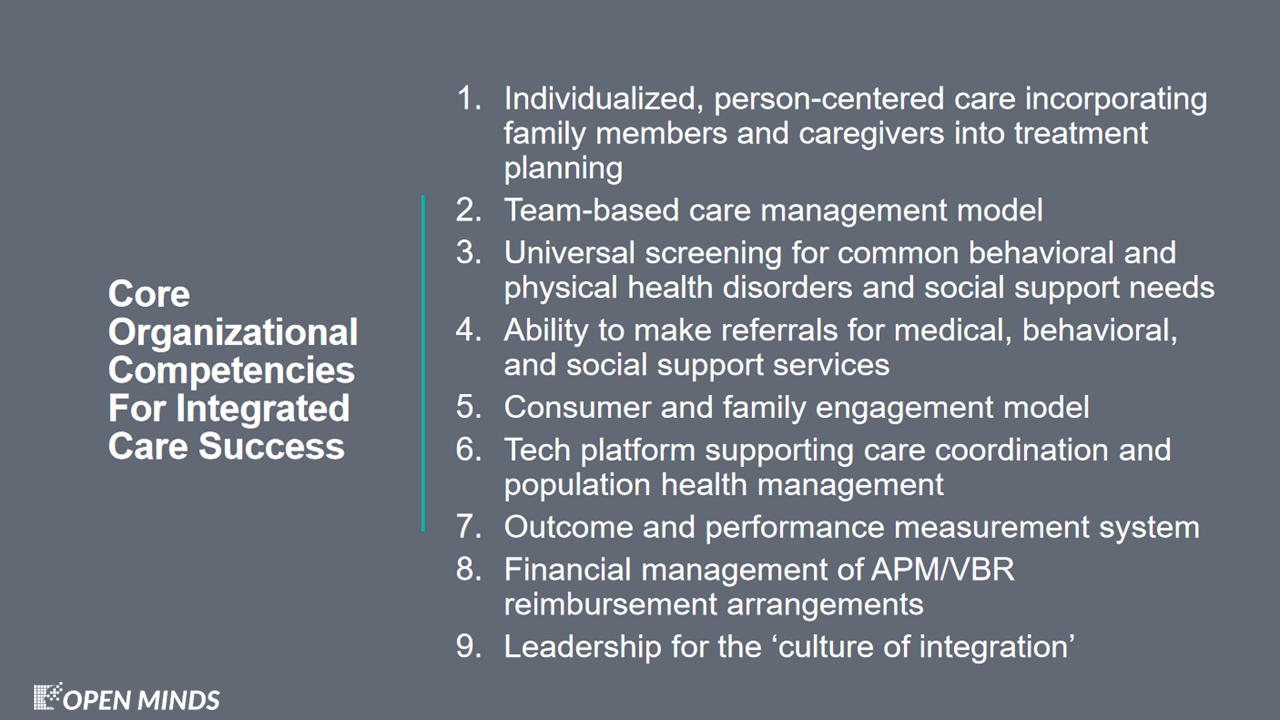
But having integrated service delivery systems does not guarantee that the participating provider organizations and their clinicians are using a whole person care model—the clinical approach looks at the whole person and considers multiple factors that impact health like social/environmental influences, health behaviors, physical health, and mental/behavioral health.
It is the totality of the view of “health” that separates the WPC approach from the integrated delivery system model. The elements of an integrated delivery systems make WPC possible. In particular, WPC depends on the standardized and prescriptive consumer referral processes based on assessments, tech-assisted referral processes, and closed-loop referral methods. While the processes may be standardized, the care plan is as unique as the consumer, their families, and caregivers.
But whether WPC will have the impact that is projected depends on whether the referrals for “behavioral health” or “social services” are actually available to consumers. The much-touted “hot-spotting” initiative of the Camden Coalition didn’t live up to is potential because of lack of community resources. The observation by Jeffrey Brenner, M.D., who founded the Camden Coalition, pointed out the fundamental issues: “The bottom line is, we built a brilliant intervention to navigate people to nowhere..”. The lack of identified behavioral health and social service needs—housing, addiction treatment, and mental health services—were not available. WPC assessments and referrals don’t have much of an impact if there are no services to refer to.
I remain optimistic about WPC—and how it will (eventually) force a reconsideration of the concepts of “health” (and of “total cost of care”). But in these early stages of this evolution, it is important to design the clinical processes and reimbursement with a best practice framework in mind.
