Health plan performance and how it is measured continues to keep the attention of executives in the health and human service field. Just in the past month, many health plans have been touting the achievement of their recent health equity accreditation, for example, Anthem Blue Cross And Blue Shield, Earns NCQA Health Equity Accreditation Plus, and Amerigroup Georgia Earns NCQA Health Equity Accreditation Plus.
More substantially, two Centene Medicare Advantage plans had enrollment suspended by CMS due to low scores. Elevance challenged their star ratings and won the challenge.
At the same time, the current value-based contracts with provider organizations focus on health plan financial performance measures like access to care, readmission rates, and emergency room use. In The OPEN MINDS 2024 Performance Management Survey of Health and Human Services organizations, 59% of specialty service provider organizations and 90% of FQHCs report participating in Value-based Reimbursement (VBR) arrangements.

Performance metrics are, for these many obvious reasons, important to health plan executives. But there is a disconnect between what executive teams of provider organizations decide to measure and what health plan managers seek. A recent survey found that most hospitals and health systems remain focused on traditional, transaction-focused metrics rather than patient-centric, relationship-focused metrics.
For executives interested in developing or expanding new models of care coordination—like health homes, enhanced care management (ECM), community supports, and in lieu of services and settings programs (ILOS)—a plan (with enhanced tech capabilities) is needed to measure, report, and manage these new metrics. This journey to technology-enabled performance management was the focus of the session, Preparing For CalAIM—Creating The Tech Infrastructure Needed For Success In A Population Health & Performance-Based Service Delivery System, held during the 2023 OPEN MINDS Technology & Analytics Institute.
Panelists included executives from Masada Community Mental Health Services (Chief Quality & Compliance Officer Iva Svetlikova, MS, LMFT; Masada Chief Development Officer Patricia Tindbaek, MSW, LCSW; and Director Of Information Systems & Analytics Khai Nguyen, MS, LMFT), California Health Collaborative (CalAIM Director Dr. John Bodtker, MPH, PharmD; Pacific Clinics Senior Vice President of Clinical Administration Gordon Richardson, MSW, LCSW) and Pacific Clinics (Vice President of Outcomes & Evaluation, Business Analytics & Training Scott Fairhurst, Ph.D.; and Pacific Clinics Director Of Outcomes & Evaluation Daniel Lakin, Ph.D.). During the discussion, three key themes emerged—understanding the technology needs for enhanced care coordination, the necessity of secure health information exchange, and competencies in leverage performance and quality analytics.
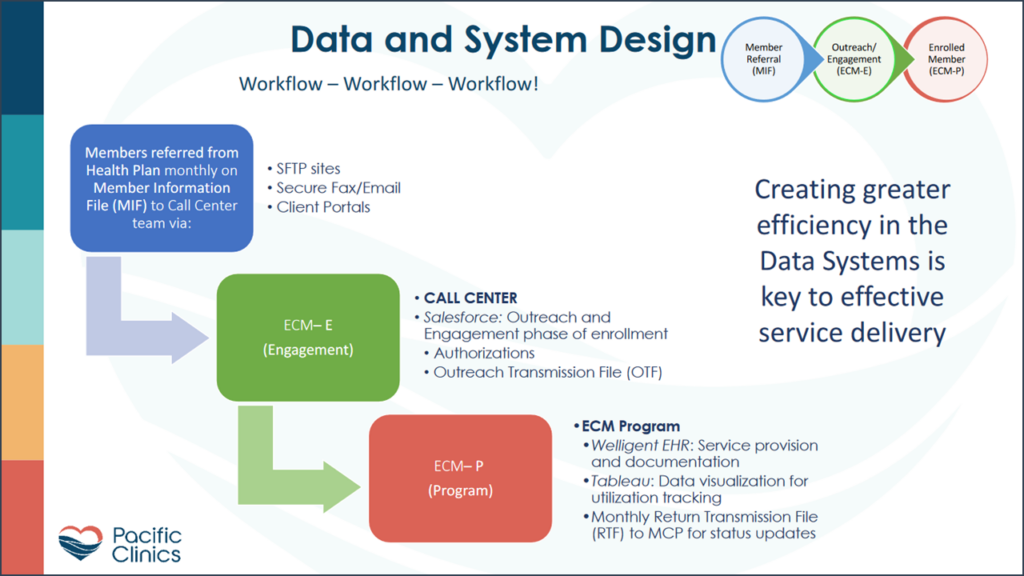
The Technology Needs For Enhanced Care Coordination Moving from a provider of services to a coordinator of services brings new requirements for provider organization—both in the technology infrastructure supporting workflows and in performance reporting. A few of the new requirements include a comprehensive longitudinal view of consumer patient health, technology-enabled care management workflows, and integration of consumer engagement and referral processes. Mr. Nguyen noted, “The technological alignments create a cohesive ecosystem that supports secure communication, comprehensive data integration, real-time monitoring, patient-centered care, and addresses functionality gaps. This alignment meets the requirements of CalAim and facilitates the successful implementation of enhanced care management.”
Pacific Clinics’ executive team found the best solution to acquiring the technology needed wasn’t a one-size-fits-all approach. They integrated solutions from a variety of vendors to create their platform. Mr. Fairhurst said, “As we were doing our strategic plan, we came to recognize that any data that we would need, whether it be to measure our cost per unit to measure our productivity, or to prepare ourselves for value-based care, it could not come from any one source system. Our strategy really centered on creating a data lake or data warehouse or multiple data warehouses”.
Secure Health Information Exchange Requirements One of the core requirements—and core challenges—of moving to a care coordinator role is having real-time access to the consumer’s longitudinal record—for health care, pharmacy, behavioral health, and social support needs. Secure interoperable processes to exchange consumer data is key to making this happen.
In California, in 2024, California’s Health and Human Services Administration established a Data Exchange Framework. This establishes a first-ever statewide unified data-sharing agreement among all private and public stakeholders. Through common data-sharing agreements and standardized policies, every California health care provider organization has access to essential information for delivering services using state-defined data-sharing pathways. Dr. Bodker states, “This platform has interoperability with other health plans and providers so it can interface with the EHR systems, the community, health information exchanges, laboratories, anything else we can get access to, so we’re working in that direction.”
Competency In Data-Driven Decision making The collection of data for performance and quality analytics is one part of the equation for success in care coordination roles—but the ability to use that data to improve services delivery and consumer outcomes is the other. For success with contracts with performance incentives and value-based reimbursement, real-time reporting of key metrics and the ability to interpret and act on those metrics is key. As Ms. Tindbaek says, “Investing in the right technology is crucial for service providers to effectively participate in the new data exchange framework and deliver quality care.”
These leaders made it clear that technology has been key to their success with the CalAIM initiatives, even as each has transformed in different ways and on different timelines. Dr. Fairhurst spoke to the significance of technology for improved care coordination, improved patient experience, improved quality, and reduced costs, reflecting, “It’s about the Triple Aim. And the Triple Aim is about balance. Can you help people get better? Can you reduce the costs? Can you help them be satisfied with the process?”
