Payers are embracing whole person care models and integrated delivery systems, and many are moving ahead with reimbursement policies to address health-related social needs (HRSNs). Since the changes in CMS Medicaid policy last year, there are now 18 states that reimburse for housing support services; 8 have nutrition support; 5 have employment support; 5 have medical respite; and 10 have infrastructure funding to support the implementation and delivery of new services. In addition, 16 states have more waivers pending.
The headlines of the past few months illustrate the trend. Nevada’s first-ever statewide “health improvement plan” identified both gaps in care and recommended new policy goals for how the state addresses SDOH. Oklahoma announced that it was adopting a closed-loop electronic referral system to coordinate electronic referrals for SDOH, including food, shelter, and transportation. In addition, Arizona, California, DC, Hawai’i, Maryland, Massachusetts, Minnesota, North Carolina, and Washington are participating in a federal initiative to reduce homelessness by addressing health-related social needs (HRSN) for housing-related services.
But like many innovative directions in health care, the concern is how to make these pilot programs a permanent part of the health and human service landscape. We got a firsthand answer to this question in the OPEN MINDS Executive Roundtable, Rapid Social Care Delivery System Evolution: The Partners In Care Foundation Case Study, featuring June Simmons, President and Chief Executive Officer at Partners In Care Foundation.

Founded in 1997, Partners in Care Foundation is a $30 million non-profit that builds community networks to provide access to social services for diverse populations with chronic conditions. Partners in Care contracts with health plans—and sometimes with health systems—to provide care management and home and community-based social services.
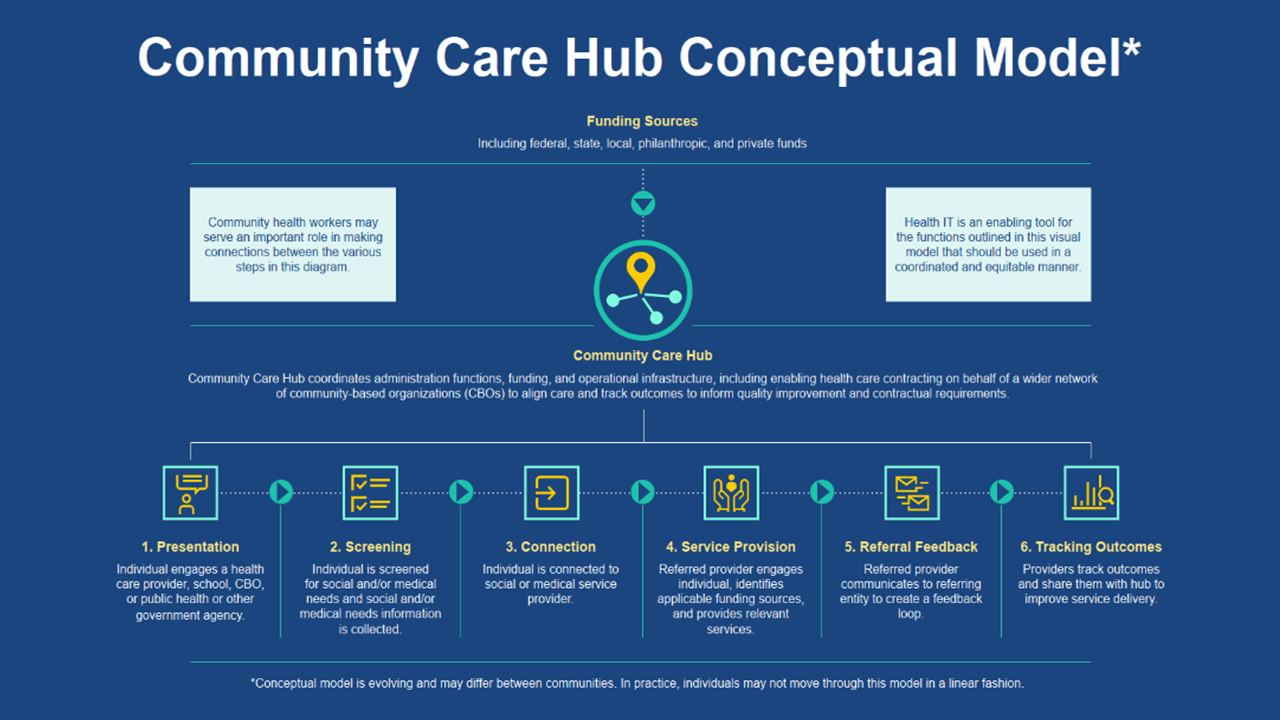
Central to this is the Partners In Care Community Care Hub (CCH) model functions. The CCH is the entity that organizes and supports a network of community-based organizations (CBOs). The CCH centralizes administrative functions and operational infrastructure, including contracting, payment operations, referral management, service delivery fidelity, compliance, technology and information security, data collection, and reporting.
Ms. Simmons discussed the three key initiatives that federal agencies are taking to support whole person care models and the provision of health-related social services. One is expanding data gathering and sharing, promoting interoperability among health care, public health, social care services, and other data systems. Another is supporting ‘community backbone organizations’ with infrastructure to link health care and community-based organizations.
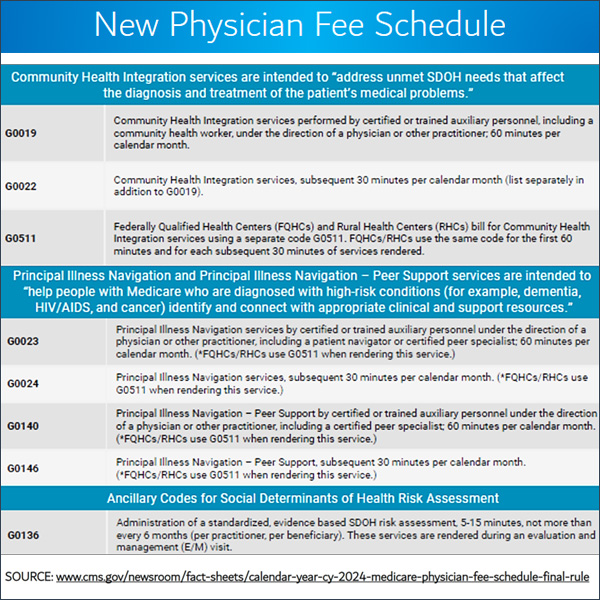
The third initiative is providing flexible funding to provide reimbursement for provider organizations to address consumer HRSN. This is happening through the Medicare Shared Savings Program Advance Investment Payments to build infrastructure and capacity to address SDOH, particularly in underserved and rural areas. And in Medicaid through Section 1115 demonstrations; Medicaid managed care programs through “in lieu of” services; and housing and nutrition supports provided under home and community-based services (HCBS) authorities. In addition, Ms. Simmons noted that the 2024 Medicare physician fee schedule added payment to clinicians for addressing HRSNs during evaluation and management visits, behavioral health visits, and annual wellness visits.
As provider organization executives look to position their service lines for success in an era of whole person care, Ms. Simmons said there are some core capabilities that are essential. Topping her list are screening tools, evidence-based practices, and partnerships.
Screening tools According to Ms. Simmons, any provider organization that addresses consumer health care needs relies on some type of standardized needs assessment. Addressing SDOH is no different. To effectively provide service or efficiently refer consumers to the right services, provider organizations need a method to identify HRSNs that can be used as part of a comprehensive management plan.
“These are people who need this service, and you have to find them and serve them well,” said Ms. Simmons. “First you have to find people and that’s not so easy. Second, you have to talk to them and you have to get them to see that you can be helpful to them. One of the ways to find people is in care transitions. There’s also growing interest in finding people in care settings. It’s beginning to be looked at as a quality measure along with health equity, accreditation, and other factors so hospitals and health plans are now required to identify social needs.”
Evidence-based intervention Evidence-based interventions are critical to providing consumer services that result in better outcomes. And it is the outcome data that is critical to health plan reimbursement. Traditionally, health plans have been resistant to contracting for social services and have paid little for those services. Having interventions with scientific evidence of a positive effect on health outcomes is critical.
PartnersPartnerships Health plans are looking for provider organizations with a whole person approach to care. To fill that needs, provider organization executive teams need to determine if they can be the entire solution. More often than not, a provider organization cannot address all of a consumer’s medical, behavioral, and social needs—and a partnership with other organizations can make that happen.
“It’s not new, but to transform in this changing environment, it takes strong partnerships,” said Ms. Simmons. “It takes interdisciplinary and cross-sector teams where health plan care managers, medical providers, hospitals, emergency rooms (ER), and community-based organizations are brought together. How do we find the people in need who will really benefit from these new kinds of approaches?”
Enterprising executives who can embrace the SDOH opportunity can position their organizations for new health plan relationships and new revenue. Success, as in most things in health care service delivery, will hinge on driving better outcomes at lower costs while having the results to prove it.
