Raised in a Swedish household, I grew up with melodious tunes from our many family accordions. (And when I left Minnesota, I developed strange affections for “Weird Al” Yankovic, Cajun zydeco, and Mexican Tejano music). The physics of an accordion is interesting in that music is made by expanding and contracting the bellows—that expansion and contraction happening regularly.
As I was looking at the Medicaid enrollment figures, they reminded me a bit of an accordion—with swings in enrollment that health and human service executives track very closely. Enrollment expands and contracts based on both federal policy and state decisions about Medicaid expansion and eligibility criteria.
Over the past six months, the new developments in Medicaid enrollment have been two-fold. There was a great increase in Medicaid enrollment during the pandemic due to some temporary eligibility rule changes. But those rule changes have almost been totally ‘unwound’ over the past six months. The other development is the continual drama at the state level in those states that recently decided to expand Medicaid—or not.
At its post-pandemic peak, Medicaid enrollment reached 92 million people. The end of the COVID-19 pandemic, also came the end to the continuous enrollment provision that mandated enrollment in Medicaid for those who lost employment during the pandemic.
Many states saw drastic disenrollment numbers. For example, in Wyoming, 17,500 Medicaid enrollees (including adults and children) have lost coverage. In Texas the coverage loss includes 2 million enrollees. As a result, the “unwinding” of Medicaid has dropped Medicaid enrollment to 84 million as of January 2024.
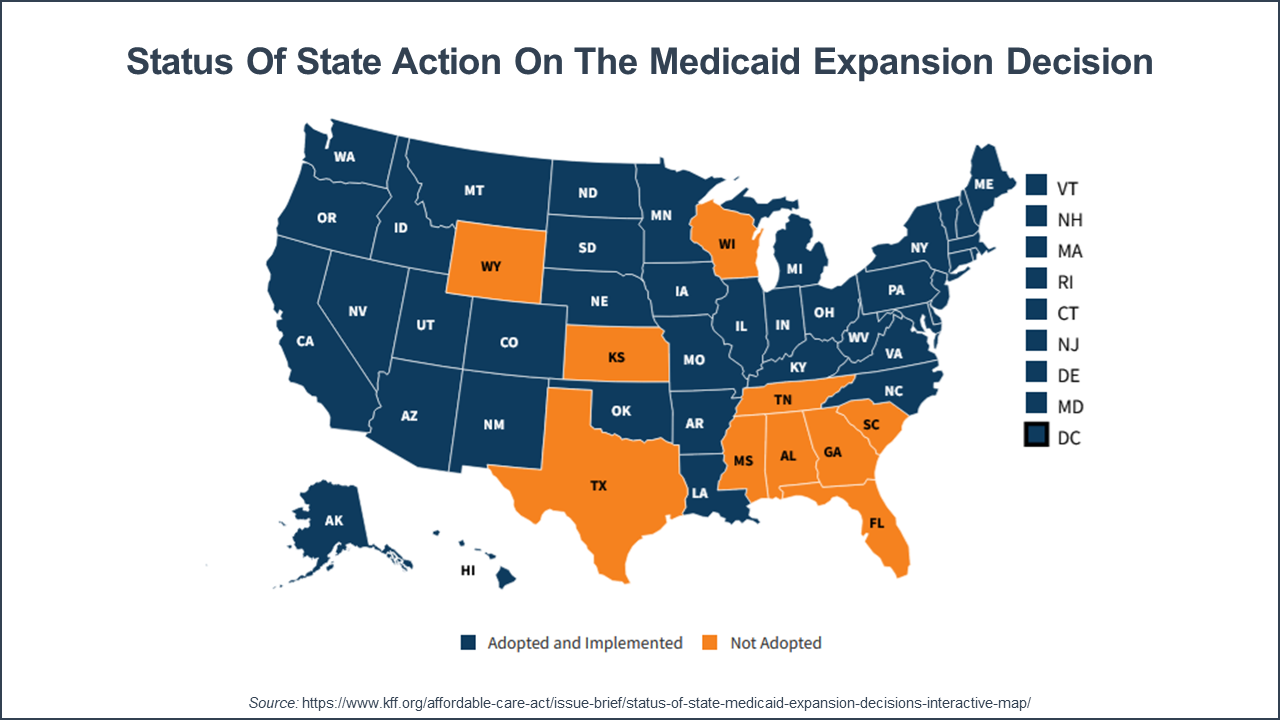
The other factor changing Medicaid enrollment is the state adoption of Medicaid expansion. To date, 41 states including the District of Columbia have adopted Medicaid expansion. As of June 2023, approximately 24.5 million adults were enrolled in Medicaid expansion. However, 10 states have not expanded Medicaid, including Alabama, Florida, Georgia, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin, and Wyoming.
In the past year, there has been Medicaid expansion activity in South Dakota, North Carolina, and Mississippi. South Dakota expanded coverage as of July 2023. And, North Carolina’s Medicaid expansion went live on December 2023. In February of this year, the Mississippi House passed Medicaid expansion legislation. However, members of the state Senate insisted on a work requirement in the program. With no compromise reached, the bill died in the legislature in early May.
It is likely that this ‘cyclical churn’ in Medicaid enrollment will continue. Since it is a state-run program, state politics will always shape the program—not just enrollment criteria, but benefits and delivery system models. And the national situation also changes Medicaid enrollment—with periods of weak economic strength increasing the number of Medicaid beneficiaries.
As of 2024, the Medicaid and CHIP programs served 25% of the U.S. population. And the program is the sole U.S. funder (apart from a small proportion of private long-term care insurance plans) of long-term care services. All of which makes Medicaid an essential and significant funder of the U.S. health care system.
