By Monica E. Oss, Chief Executive Officer, OPEN MINDS
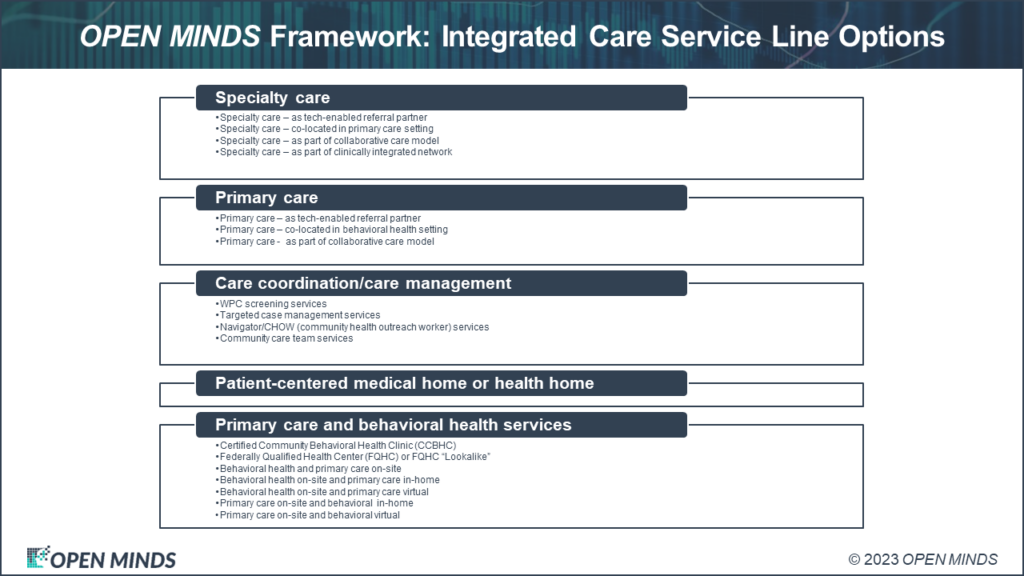
“Every health and human service organization needs an ‘integration’ strategy.” This is the conclusion of our team of senior advisors, Christy Dye and Deanne Cornette, when we’re discussing financial sustainability, growth, and strategic plans. “Integrated care” delivered with a whole person care model, has been demonstrated to both improve consumer health status and reduce costs. And as “integrated” models of care gain favor of payers and the health plans that manage their benefits, the “trickle down” effect on strategy is felt by every provider organization.
What all integrated care strategies share is the need for interoperability—the ability to share data with other stakeholders in the health and humans service delivery system. Real time, automated data sharing is crucial for reducing service duplication, consumer empowerment, care coordination, and improving population health with data-driven insights.
I asked Christy Dye, who has served on the executive leadership team for Contexture, the regional HIE serving Arizona and Colorado, about the challenges organizations face trying to solve the interoperability problem. According to her, one of the critical challenges organizations face when starting the journey to whole person, integrated care is the need for data from outside of their own lower case Electronic Health Records (EHR) system to identify all the points where consumers “touch” the health care system. “If a clinician is relying on their patient to self-report their visits to the emergency room, the EHR record is likely to have large gaps. One of the most stunning moments I experienced in implementing an integrated care clinic was discovering how often our patients with serious mental illnesses reported their visits to emergency rooms. They may have reported one or two visits, but data from our local health information exchange would show 40 or more visits. This data changed the way we worked with people in their care plan. And, luckily emergency room reduction was also one of the performance measures in our health plan contract. This real-time access to all patient data through the HIE helped us improve our care and patient outcomes—and earn financial incentives.”
This need for interoperability has spawned several different types of initiatives. One of them is the creation of Health Information Exchanges (HIEs)—there are already 89 HIEs in the US. In Indiana, the statewide HIE—the Indiana Health Information Exchange (IHIE)—has been credited with reducing hospital admissions by 26 percent over a five-year period while also lowering overall healthcare costs. The system connects more than 100 hospitals across the state, enabling providers to access patient information quickly and securely. Another HIE which provides secure access to patient data from over 62,000 health care professionals in New York state has provided estimated annual cost savings of $12 million.
But data sharing is possible without an available or affordable HIE. Increasingly data systems are adopting common standards for data sharing. The challenge for provider organization executive teams is not only developing an integrated care strategy, but also developing interoperability with the health plans and provider organizations in their care ecosystem. Without this capabilities, provider organizations are limited in their ability to participate in integrated care initiatives.
As the field moves to more integrated care models—and more value-based care—expect to see more pressure for provider organizations to develop interoperability functionality. And for health plans, that want to financially align with their provider network, to create new platforms for real-time data sharing with provider organizations.
