The move to whole person care models and integrated care delivery continues. More Medicaid RFPs focus on integrated service delivery systems are being awarded with the market is likely to follow. Most fundamental is for behavioral health provider organizations to move to population health management model of service with integrated community interventions to realize value.
To accomplish this, payers and health plans need to change provider reimbursement with more thought to bundled and capitated rates that support integrated delivery. The data on the value—in terms of outcomes and cost—is pushing this movement. As a result, every executive team of a specialty provider organization needs an integration strategy—and likely more than one.
For markets and payers that are at the start of the performance and value contracting journey, that strategy could be as basic as interoperability of consumer data and strong referral relationships. In more advanced markets, it could be forming a clinically integrated network (CIN) or creating an integrated physical/behavioral health service model.
The formula for provider organization success in an integrated health landscape was the focus of the recent session, Building A Successful Clinically Integrated Network (CIN): The Roadmap To Long-Term Value. The session was led by Seth Terndrup, Senior Vice President of Legal Affairs with Alera Health. Alera Health, through provider-led ONEcare Networks, operates clinically integrated networks in five states. These ONEcare Networks include nearly 15,000 clinicians and provide services for 3.6 million members.
The CIN model is an integrated care strategy option, particularly for community-based provider organizations that want to both maintain their independence and share infrastructure for managing integrated care contracts and value-based reimbursement. By definition, a CIN is a collaborative system that brings together all clinical providers—specialty care and primary care providers, inpatient facilities (hospitals, clinics), and other hands-on caregivers to coordinate care to improve outcomes and control costs (value).
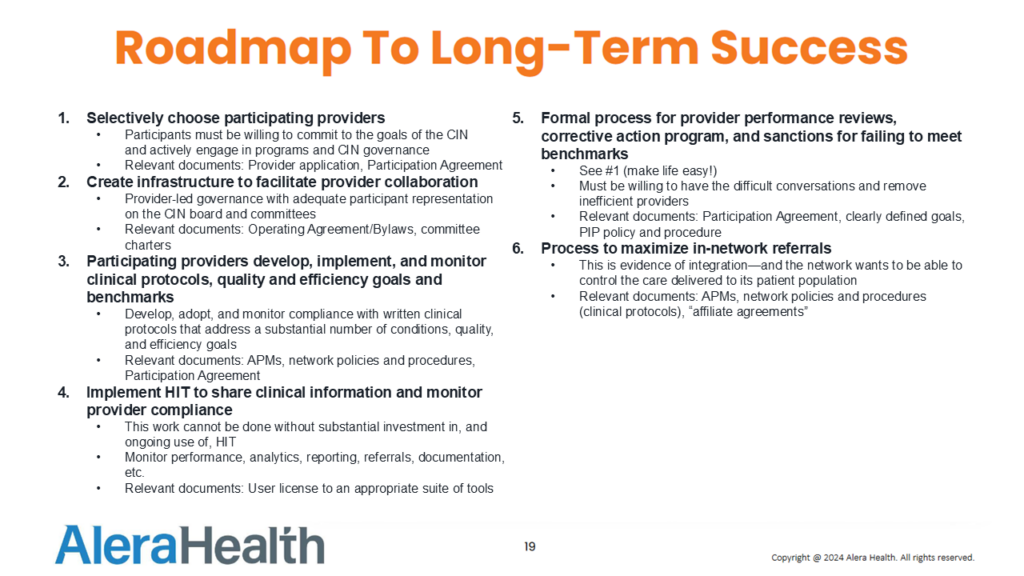
Mr. Terndrup provided great advice to executives working to perfect their integrated care operations—from partner selection to human and technology infrastructure to shared clinical protocols and a continuous quality improvement process.
Partner selection in integrated care: The steps to become a clinically integrated network through a CIN structure are ongoing, not one and done, according to Mr. Terndrup. “The participants that enter your network need to be willing to coPartner selection in integrated care: The steps to become a clinically integrated network through a CIN structure are ongoing, not one and done, according to Mr. Terndrup. “The participants that enter your network need to be willing to commit to the network’s goals,” he explained. “They need to be actively engaged in the programs and in CIN governance.” A written operating agreement or bylaws, and committee charters are a must. There should be a committee structure to ensure the network’s quality and efficiency goals are implemented and monitored and the participants’ financial incentives are aligned with those goals.
The human and technology infrastructure to make integration work: As with everything in delivery today, the CIN will require a robust information technology system to share information across the provider network. The network will require a means to collect and analyze population and patient level data, coordinate care, send and receive referrals, and communicate with care team members. A robust technology system is also vital to monitoring provider compliance with the network’s clinical standards and for measuring performance. “The work of clinical integration cannot be done without a substantial investment in technology,” said Mr. Terndrup.
Shared clinical best practices and clinical decision support: A CIN is expected to operate under written clinical guidelines to ensure clinical quality and efficiency. Maximizing in-network referrals, in an appropriate manner, is necessary to control care delivery and effectively advance the network’s cost and quality goals. Another critical component is a formal process for provider performance review, which includes corrective action for under-performance.
A data-driven continuous quality improvement process: At its most basic, a CIN leverages and improves quality among disparate providers into one effective unit. Data collection, verification, and analysis must be in place to measure such efficiencies. Among operational considerations, the documentation end are mental health screenings, often associated with worse medical outcomes, cognitive behavioral therapy to treat depression and anxiety, and screening to determine how social determinants of health (SDoH) stressors impact both physical and mental health. These therapy reports must be shared across all providers to support continuous quality improvement within integrated care.
Mr. Terndrup’s big takeaway was caution around the legal setup of CINs. Any integrated model must be based on advice from experienced legal counsel, as it’s easy to get it wrong and violate antitrust laws. Ultimately, a CIN cannot be established solely to obtain better rates through joint negotiation; the primary goal must be cost reduction and quality improvement. For example, a CIN cannot be established to suppress competition unreasonably. However, providers need to be appropriately incentivized to invest in this work. Often, those incentives can only be achieved through joint negotiation under a carefully structured CIN. He also stressed that some states have their own requirements that must be met prior to establishing and operating a CIN. In conclusion, Mr. Terndrup offered this insight. The definition of a CIN is open-ended. “There are shared goals between providers and payers (in a) value-based environment. If you put …success together on a daily basis, month after month, year after year, you start to have what looks like real industry change. So that, in my mind, is CIN success.”
