By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Federal initiatives to achieve information interoperability in health care have been a mixed bag. The initiative brought most provider organizations to the point of having an electronic health record keeping system, but widespread standard information exchange has been elusive.
But “integrated” care coordination models (crossing medical, behavioral, and social domains) and whole person care approaches are essential for most provider organizations for long-term sustainability—and both require information exchange. The strategic question for most provider organizations is how to make that happen.

We got an up-close look at how one provider organization, COPA Health in Arizona, is making that happen in the session, Turning Artificial Intelligence Into Actionable Intelligence. The session was led by Dr. Michael Franczak, Director of Population Health at COPA Health during The 2022 OPEN MINDS Care Innovation Summit at The 2022 OPEN MINDS Executive Leadership Retreat.
Dr. Franczak described how COPA Health is leveraging their technology investments, including their EHR, using tech tools to improve their ability to be proactive with consumers, and manage the populations of consumers in their care. He described a three-phase evolution of their use of tech tools, from artificial intelligence (AI) to assisted intelligence to actionable intelligence.
Use of artificial intelligence: AI is at the core of using the management of data to improve outcomes. And that process begins with the ability to merge disparate data sources and do basic analyses of what it says. “We take the data and put it in a ‘data lake’”, said Dr. Franczak. “The data lake has different types of information coming into it and some of it is muddy. Not everything connects with everything else perfectly. That’s where you need analytic folks to be able to see how you can match this with that. Everything then comes together in a product that we’ve developed called Nexus. We then have files that contain everything that’s happened with respect to what one sees for a population, for a clinic, for a provider. We are combining real time reporting as much as possible. We’re bringing in scheduled reports, email, we’re using panels and data on risk lists and member surveys. Part of the data that we bring in we use to develop risk stratification.”
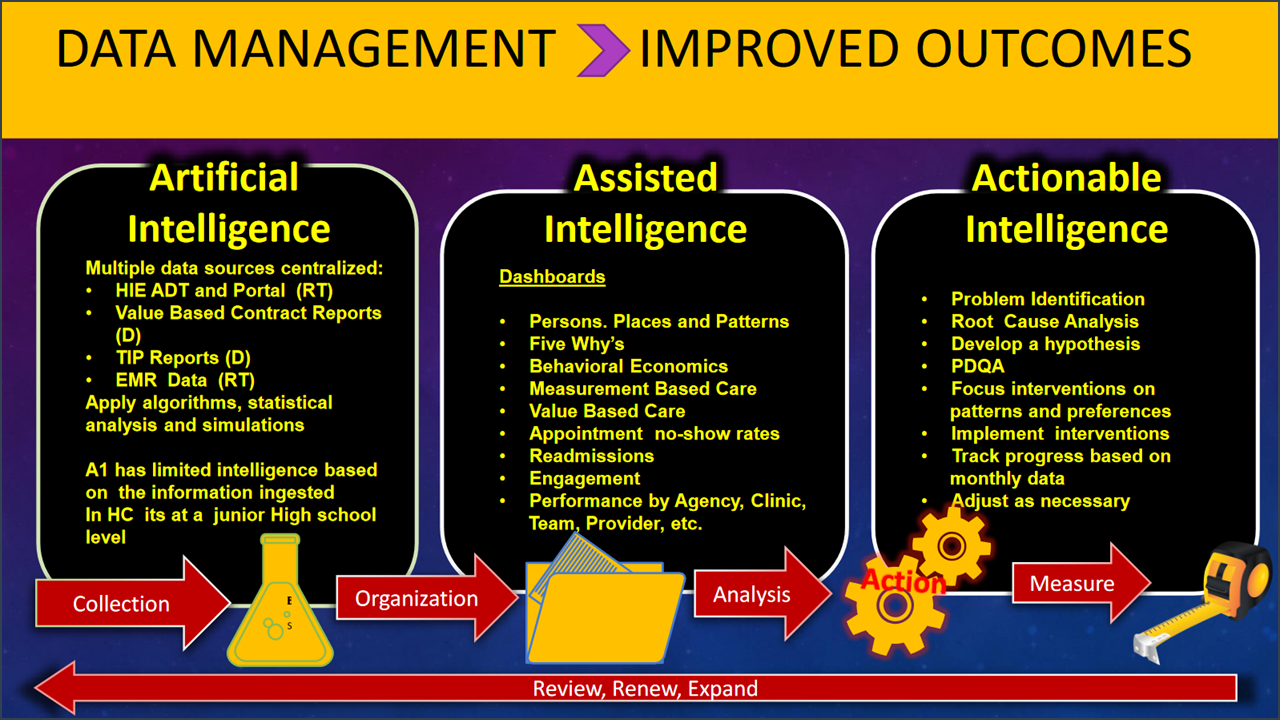
Use of assisted intelligence: While the rudimentary use of AI speeds the tasks conducted by staff, assisted intelligence helps staff improve the effectiveness of their activities. “We take basic data and take it to assisted intelligence,” said Dr. Franczak. “And what I mean by that is we take the data that is needed by the team and we have brainstorming formulations to figure out what’s going on with a particular case. We had a guy with 95 ER visits and did an analysis to figure out why. We facilitated a meeting of the clinician who knows the person and one of my first questions is, who knows this person best? And it’s not the most highly credentialed person. But it could be. It could be anyone on that team who’s made a connection through engagement with that individual.”

Use of actionable intelligence: In the final stage of evolution of the advanced use of data, the actionable intelligence stage provides insights that staff would not have had without the advanced analysis of data. “A lot of data in your EHR is unusable without sitting there with people who wrote the notes,” said Dr. Franczak “We take that data and try to make it actionable, which means we do a root cause analysis to determine what’s driving the issue. For example, if you’re finding someone going in and out of hospitals, and the reason is not that they have untreatable or unstable psychosis, self-injury or self-harm, or are gravely disabled, then you have to look at what’s driving the behavior. We often find out, they lost their home, they’re couch surfing, they just got kicked out of their grandmother’s house. And we found that many of the individuals are using hospitals as a survival mechanism because of their current circumstances.”
In most areas of commerce, including health and human services, the competitive advantage and success will go to the organizations that have the team and infrastructure to best leverage available information. Since widespread interoperability is the exception rather than the rule in the field, executive teams are looking for tools to integrate data and metrics-enabled decision making at the organizational level. That will likely be the plan for most organizations for the foreseeable future.
