By Monica E. Oss, Chief Executive Officer, OPEN MINDS
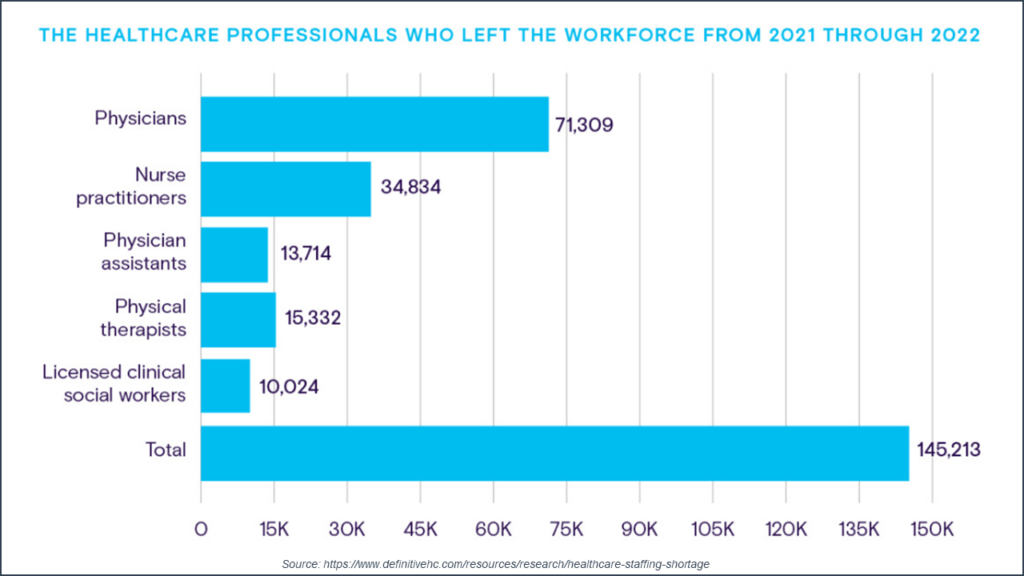
Finding clinical talent remains a strategic challenge for health and human service organizations. And this challenge is fueled by record numbers of clinical professionals leaving the field. In 2022, a total of 145,213 health care professionals left their jobs. The greatest numbers were in physicians and nurse practitioners, with over 71,000 and 34,000 professionals, respectively, leaving the field between 2021 and 2022. This is 6% of the physician workforce and 9% of the nurse practitioner workforce. During the same time, over 10,000 clinical social workers moved to other fields.
The analysis also noted that the clinical professionals most affected by workforce shortages include internal medicine physicians, family practice physicians, clinical psychologists, psychiatrists, and pediatricians. Workforce shortages in these disciplines are attributed to retirement, pandemic-induced burnout effect, and requirements for face-to-face consumer interactions.
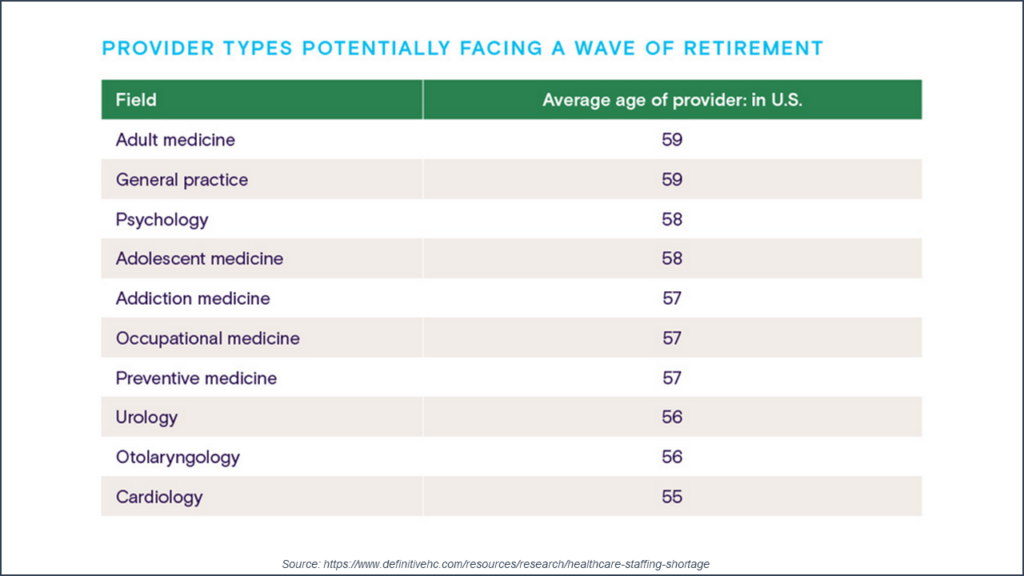
In addition to the issues of professionals leaving the field, the retirement issue looms large in the health care clinical workforce. Nearly 45% of physicians are older than age 55, and more than 40% of active physicians will be 65 or older in the next ten years. The average age of the workforce in many disciplines is over 50. Notably, the average age of psychologists is 58 and the average age of addiction medicine physicians is 57.
The health system problems created by the shrinking number of clinical professionals are many. There is lost revenue due to inability to staff positions. Increasing labor costs with the rising compensation rates for key clinical team members is another. Increases in medical errors have been documented. And there is a loss of knowledge, and resulting poorer quality of care, with large departures of clinical talent.
The question for managers of health and human service organizations is how to plan for and mitigate the effects of this dearth of clinical talent. One strategy is to embrace hybrid service delivery—with more use of telehealth and tech-enabled in-home service delivery. Telehealth and remote patient monitoring devices can help clinical professionals by automating the collection, analysis, and sharing of consumer health data. This decreases administrative time and also leverages the productive time of clinical talent.
Beyond hybrid service delivery, managers can also leverage technology and AI for a wide variety of functions. Technology can assist in diagnostics, in treatment planning, and in supplementing some therapies. And tech support for administrative processes like scheduling and documentation can further leverage clinical talent.
Finally, at this point in time, management teams should look at how best to assess the causes of burnout—and embark on systematic changes to address those causes. This could include creating a culture that fosters staff resilience, fair leave policies, safe and secure working environments, processes for shared decisionmaking, adequate benefits, and fair leave policies.
For health and human service organizations, there is little value proposition for consumers or payers without high-performing clinical staff. The numbers on the shortage of talent are clear. The key for executive teams is thinking through how best to design and deploy new tech-enabled service delivery systems that will benefit the clinical teams and consumers they serve.
