
By Monica E. Oss, Chief Executive Officer, OPEN MINDS
We’re awash in more and more data. The question is how to turn that data into information for organizational strategy—information that can improve performance. For health and human service plan executives, competitive advantage is dependent on developing tools that prompt real-time decisions. And according to UPMC Health Plan Vice President and Chief Medicare Officer, Angela Perri, in her keynote session Leading A Technology Transformation—Tech & Analytics To Improve The Consumer & Clinical Professional Experience at The 2021 OPEN MINDS Executive Leadership Retreat, that real-time decisionmaking becomes more meaningful when systems move beyond predictive analytics to adaptive analytics.

Adaptive analytics is real-time data capture and analysis of data that provides insights for immediate adjustments. The goal is to bring together claims data, clinical data, and consumer feedback data in a way that enables consumers and their clinical advisors to make decisions about current and future treatment.
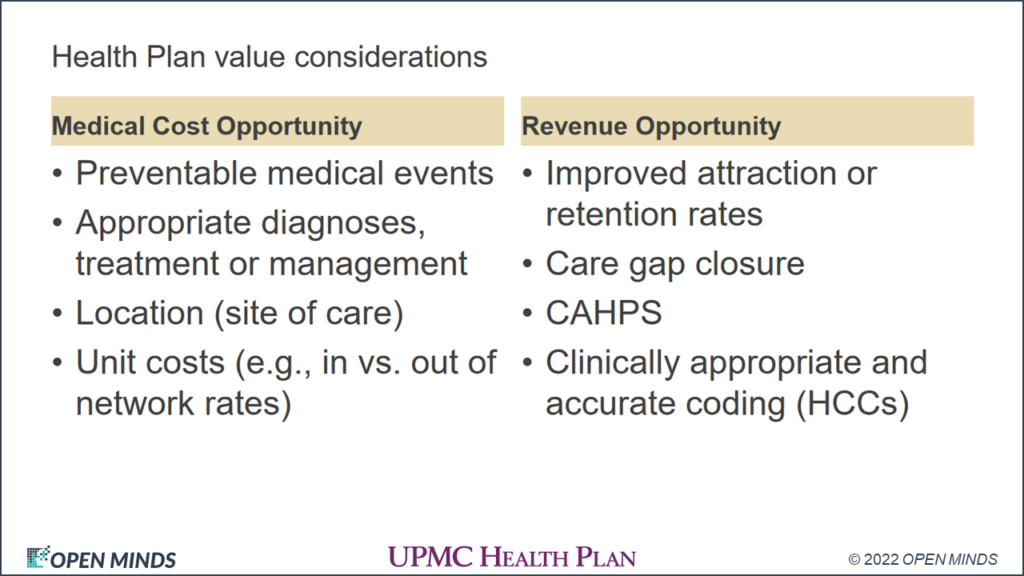
Adaptive analytics can be a key to success in value-based relationships between health plans and provider organizations. By facilitating bidirectional data sharing between health plans and provider organizations, and sharing that data with consumers, all three stakeholders have access to the same critical information. Health plans are better informed of the consumer and their treatment needs. Provider organizations and their clinical professionals have the data needed to understand and monitor key value measures about both medical costs and revenue opportunities.
But this type of bidirectional data sharing is the exception rather than the rule right now. The questions are what is needed to make this happen—and what is the timeline? From a technical perspective, this happens more piecemeal, with the sharing of data from health plan claims systems, provider organization electronic health recordkeeping systems (EHR), and any other consumer data sets using application programming interfaces (APIs).
According to Ms. Perri, she envisions this all happening in the next five years. “I’d like to see it in three,” she said. “Every health plan has a different focus overall and even if the infrastructure from a plan perspective isn’t where it needs to be, the investments is there.”

That might seem like an aggressive timeline, but the consumer-centric use of data was accelerated during the COVID-19 pandemic as well as Centers for Medicare & Medicaid Services (CMS) interoperability and transparency rules. The health and human service system has stakeholders at every level seeking an “Amazon-like” platform. Consumers want all of their personal health data in one place immediately—with opportunities for “self-service” on both the administrative side of health care and in managing their own care.
There is one practical issue. Will the tool sets and interoperability that evolve over the next few years be unique to each health plan? Will this force provider organizations into nearly exclusive relationships with the health plans they work with? To be successful, Ms. Perri stressed that this can’t be about the tools. “It’s about driving the outcomes differently,” she said. “If we have tools that are exclusive to just us, will you use that if you are [also] working with other health plans? That’s how it’s been, but I don’t think that’s sustainable. Tech changes too fast. I think this will be more agnostic in time, however the greater challenge will be impacts to privacy should multiple third-party applications not held to HIPAA or other standards be used by consumers. They likely won’t realize what they are giving away in fine print until it’s too late.” Nonetheless, movement toward greater sharing of relevant or actionable information will be the key to the best outcomes and consumer satisfaction.
