By Monica E. Oss, Chief Executive Officer, OPEN MINDS
One-in-three Americans have medical-grade diagnostic technology, ranging from wearable continuous glucose monitors, to watches and smartphones with various sensors to measure physical and mental wellbeing. These devices, along with telehealth capabilities, are helping organizations further extend their reach into communities to facilitate whole-person care, while also reducing congestion in emergency departments (EDs) and inpatient facilities.
And remote monitoring technology is making hospital-at-home care a practical option to facilitate whole-person care. In one study, consumers receiving hospital-at-home care had lower depression and anxiety scores, and had a 26% lower risk for readmission and a lower risk for long-term care admission relative to the in-hospital group.
We discussed the value of wearables and medical devices and how analytics are a vital technology for whole-person care. That can enable organizations to identify interventions that can reduce mental health crises and direct consumers to the appropriate crisis resource at The 2024 OPEN MINDS CEO Technology Summit in the session Using Technology As A Means To Enrich Clinical Outcomes: How A Whole Person Care & Crisis Program Are Creating New Quality Standards In A “Digital-First” Age, featuring Margie Balfour, MD, Ph.D, Chief of Quality & Clinical Innovation, Connections Health Solutions, and Hossam Mahmoud, MD, MPH, Regional Chief Medical Officer, Carelon Behavioral Health.
Headquartered in Arizona, Connections Health Solutions LLC (CHS) specializes in behavioral health crisis care and a range of services to help stabilize and treat people with mental health and substance use diagnoses. CHS has two locations in Arizona, with additional locations in Montana, Pennsylvania, Virginia, and Washington. CHS has secured $58 million in funding from Town Hall Ventures and Heritage Group.
CHS’s approach to whole-person care is called the CRISES Framework, and its goal is to deliver high-quality services that are timely, safe, accessible, least restrictive, effective, consumer and family-centered, and to leverage partnerships when applicable. Metrics collected on these areas include internal key performance indicators and quality metrics, partnership metrics, outcomes metrics, system outcomes, and research metrics.
The result is that CHS can track the flow of a consumer in crisis throughout the system. For example, a recent CHS data analysis shows that 57.4% of crisis episodes began with a mobile crisis team or at a crisis facility, rather than at the ED or an inpatient clinic. Of those, 69.1% remained in the crisis system, ending with a mobile crisis team or at a crisis facility. Among these consumers, 63.3% did not reutilize any services within 30 days, and for those who did reutilize services, 73% did so in a crisis setting, instead of the ED or at an inpatient clinic.
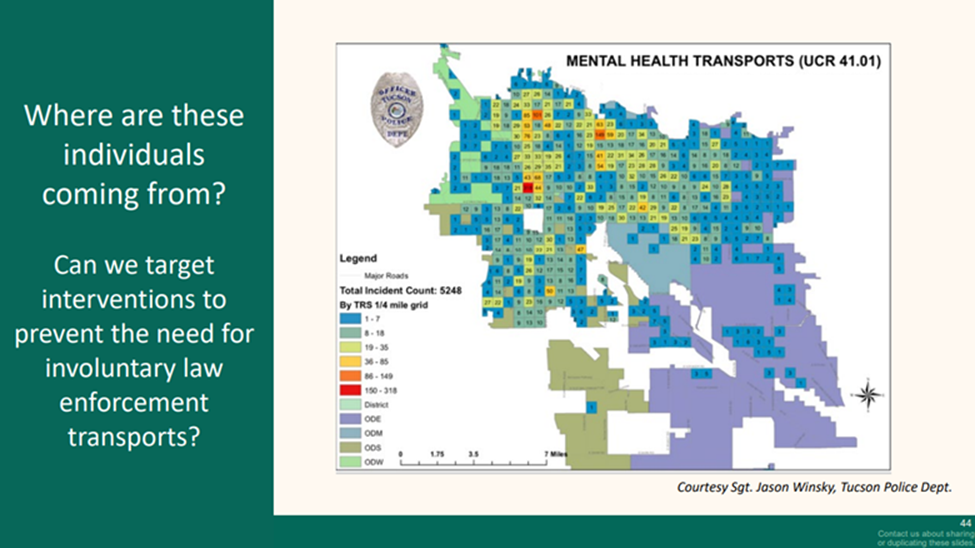
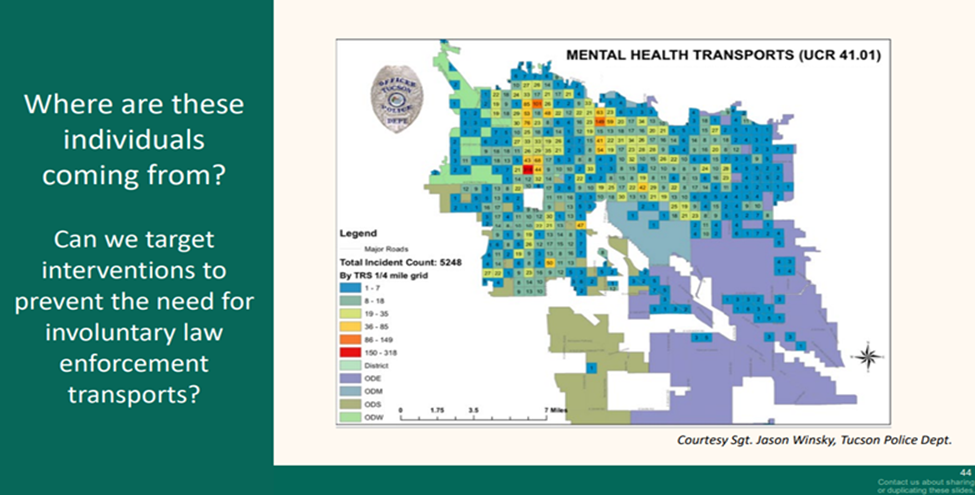
For consumers who enter a CHS crisis setting, CHS tracks where they reside within the community, so interventions can be deployed—such as educational programs, housing assistance, substance use mitigation—to prevent behavioral health crises or lessen their severity.
Another organization leveraging analytics is Carelon Behavioral Health, which uses technology to create digitally enabled whole-person care programs for child psychiatry, concierge care, and maternal health. “These programs are innovative because they use technologies in different ways in the design and implementation of the program,” Dr. Mahmoud said. “They diversify choice for our members to engage either digitally, in person, or telephonically. They help us expand the workforce in a manner that’s unconventional, and they support whole health, which is an issue that we continue to struggle with because of the fragmentation in our system.”
Boston-based Carelon Behavioral Health (CBH) is a subsidiary of Elevance Health—, with more than 115,000 network providers and more than 47 million members across all 50 states. Among its behavioral health consumers, Medicaid is CBH’s top payer, representing 25 million members, followed by commercial payers (21 million) and Medicare Advantage (1.5 million).
CBH’s efforts to expand child psychiatry access began in 2004 when it helped design and implement the Massachusetts Child Psychiatry Access Program (MCPAP) for the state. The program provides pediatric physicians with free child psychiatry consultations. In addition to promoting best practices when treating children with behavioral health conditions, MCPAP also promotes optimal resource utilization for scarce specialty resources.
The organization’s concierge care program is designed to provide digitally enabled case management to address high-cost, chronic and complex health conditions. Central to this program is a custom app developed by CBH, which is personalized to the consumer’s whole health needs that can include physical health, behavioral health, prescriptions, and health-related social needs (HRSNs). Consumers can engage directly with dieticians, nurses, social workers, health advocates, and coaches. Seventy-seven percent of enrolled consumers use the app to proactively track and manage their health. To date, the concierge care program has resulted in a 14% reduction in ED visits, 24% reduction in inpatient visits, 58% reduction in ED visits for members with breast cancer, and a 25% improvement in Crohn’s disease symptoms and flares.
“The app is also a vehicle to collect patient-reported outcome measures in a manner that historically has been pretty difficult for us to do,” Dr. Mahmoud said.
CBH’s maternal health program and peer-supported substance use disorder (SUD) program, Thrive, is designed to reduce the incidence of neonatal abstinence syndrome (NAS) and neonatal opioid withdrawal syndrome (NOWS). Thrive uses predictive modeling to identify at-risk women who are contacted for screening and enrollment. Year-over-year results show that Thrive decreased the number of infants born with NAS or NOWS by 346 babies. Thrive produced a $5 million neonatal intensive care unit (NICU) cost savings in 2024.
For those looking to leverage analytics in their whole-person care programs, Dr. Balfour recommends that organizations start by answering three questions: What do you have? What did you do? Did it work? The “what do you have?” question focuses on structure—software, computers, space, staffing. The “what did you do?” question focuses on process, such as whether workflows are performing as designed so that problems can be quickly detected and improved using process engineering methods. And, finally, the “did it work?” question looks at outcomes—did the action or process result in improvement?
To select crisis system metrics, Dr. Balfour recommends that organizations create a group composed of all users and stakeholders. The group’s high-level purpose is to define and memorialize the organization’s values, goals and intended results. This is followed by mapping the component pieces of the system to determine optimal flow, assess current gaps, and define success and agree on how to measure it.
For organizations looking to develop an app to support whole-person care, Dr. Mahmoud emphasizes that consumer engagement is the key to success. Engagement strategies that worked for Dr. Mahmoud’s organization include gamifying the app to make it fun, creating achievable health and wellness goals for consumers to track in the app, and providing access to live health professionals via the app.
“It’s an ecosystem that emphasizes integration across specialties, that emphasizes following members across their journey, through care coordination,” Dr. Mahmoud said. “It’s an ecosystem that emphasizes the importance of data exchange, data analytics and predictive modeling to focus on everyone that we serve regardless of condition, and incorporates health equity in the design in order to mitigate any challenges associated with the digital divide. And, last but not least, one that emphasizes outcomes and that uses outcomes to really examine the effects and impact of our programs and reassess ways in which we can refine these programs on a continuous basis.”
