By Monica E. Oss, Chief Executive Officer, OPEN MINDS
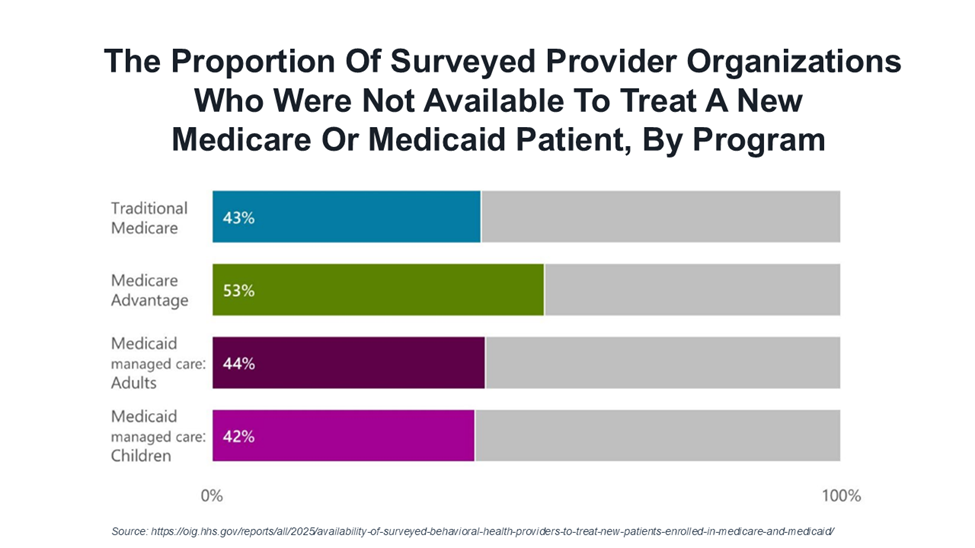
One of the problems with mental health networks? When called by ‘members,’ 45% of surveyed behavioral health provider organizations reported that they were not available to treat new consumers enrolled in traditional Medicare and Medicaid, Medicare Advantage, and Medicaid managed care—Availability Of Surveyed Behavioral Health Providers To Treat New Patients Enrolled In Medicare & Medicaid.
The new study found that among behavioral health provider organizations that could not accept new patients in Medicare fee-for-service, Medicare Advantage, Medicaid fee-for-service, and Medicaid managed care, 73% reported being unable to schedule appointments for any new patients, regardless of their insurance or payment method. Many cited full caseloads as the reason.
Additionally, approximately a quarter of provider organizations that were unable to schedule new appointments reported that they had stopped participating in traditional Medicare, Medicare Advantage, or Medicaid managed care. Some reported they had problems getting payment from the health plans.
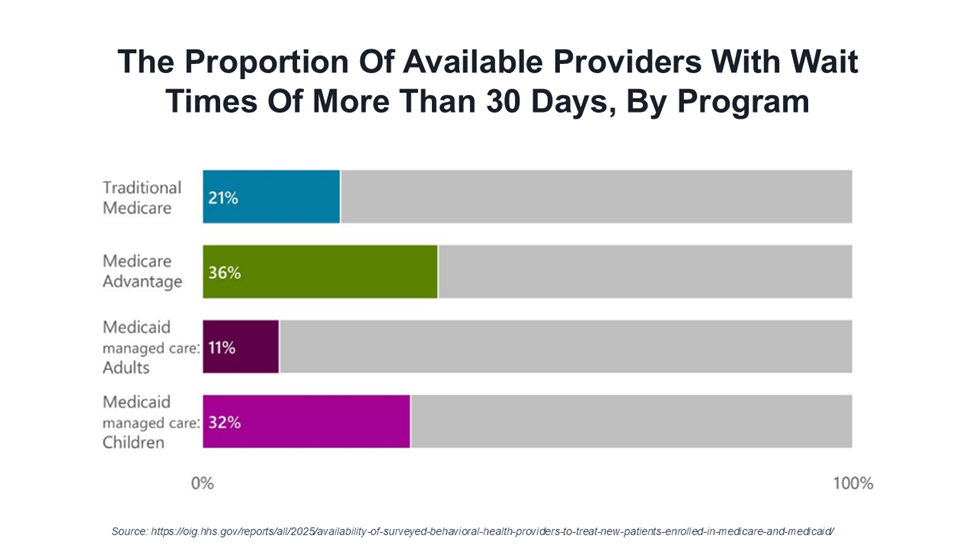
Among the 55% of provider organizations that were available to treat new patients enrolled in Medicare or Medicaid, 48% could treat a new patient within 7 days. About a quarter reported wait times of more than 30 days for an appointment.
Among those provider organizations who were available to treat Medicare and Medicaid enrollees as new patients, 53% could do so both in person and via telehealth. The wait times for in-person and telehealth were equivalent. In addition, 36% reported that a new patient’s first visit could only occur in person, and 11% of available provider organizations offered telehealth appointments only. For all of these factors, rural and urban data were approximately the same.
This access situation occurs within the context of payer health plan access standards. Medicare Advantage has a wait time standard of 30 business days for routine and preventive care, including behavioral health services. For most Medicaid managed care plans, state-developed wait time standards must be no longer than 10 business days for routine outpatient mental health and substance use disorder (SUD) appointments. The consumer access data is problematic. When consumers are unable to get ready access to behavioral health services, their use of inpatient services rises. Consumers newly diagnosed with behavioral health conditions who received timely outpatient care—such as counseling or psychotherapy—had significantly lower total costs of care over one and two years. These savings were primarily driven by a reduction in emergency department visits and inpatient hospitalizations. On average, first year medical and pharmacy cost savings occurred among people with at least three outpatient visits with a behavioral health provider organization. The savings offset the cost of the additional outpatient behavioral care, resulting in a positive return on investment.
The question for health plan and provider organization executives is how to improve behavioral health access and, in turn, reduce unnecessary emergency room (ER) and hospital use. When I broached the subject with my colleague, OPEN MINDS Senior Associate, Margaret Mays, she advised heath plan executives to expand access through multiple strategic levers. This includes increasing reimbursement rates, proactively recruiting provider organizations to grow the network, ensuring the accuracy of provider directories, and streamlining credentialing and oversight processes.
Dr. Mays emphasized the importance of aligning with the CMS behavioral health roadmap. For example, telehealth expansions are now permanent for Medicare, and there is a growing emphasis on school-based services for children on Medicaid and community-based crisis response infrastructure. She recommends that health plans invest in all three. Screening for social determinants of health and ensuring referral connections to community supports also plays a critical role in preventing avoidable crises that drive up inpatient and emergency room utilization.
And health plans should take advantage of the 2024 CMS expansion that allows marriage and family therapists and licensed mental health counselors to bill Medicare independently. “Plans need to ensure that their claims payment systems and reimbursement structures are updated to reflect these newly eligible clinicians, Dr. Mays said. “This is a critical workforce channel that can’t be overlooked.”
And there are opportunities for provider organizations to speed access to services. Dr. Mays recommends leveraging technology to improve productivity—centralized scheduling, telehealth services, and streamlining documentation processes. She also noted that in that a growing number of states—currently 38 states for both mental health and SUD—offer reimbursement for peer support services.
Finally, Dr. Mays encouraged both health plans and provider organizations to move to non-fee-for-service value based contracts for behavioral health services. Case rates and bundled rates provide the flexibility to service consumers in a variety of models with an expanded array of technology-enabled services.
While ready access doesn’t guarantee lower total costs of care, it is a necessity in making that happen. As Dawn Zieger, Vice President, Department Of Psychiatry & Behavioral Health of Geisinger, said in her session, Next Generation Whole-Person Care: Behavioral Health As Primary Care at The 2024 OPEN MINDS Strategy & Innovation Institute: “Increasing access is strategic. You can’t have quality care without access.”
