By Monica E. Oss, Chief Executive Officer, OPEN MINDS
In less than fifteen years, the U.S. health care system’s view of social services has completely turned around. Traditionally, payers and health plans were quick to draw the line between what was health and what was social. The data has always proved that social factors were major contributors to health care costs. However, there wasn’t policy support for blurring those lines or funding to pay for services that were not “medically necessary”.
But now there’s a different perspective. Over the past three years, our team has covered a range of changes in payer policy and health plan reimbursement focused on social services–and the opportunity for provider organizations to develop new services to meet those needs. An example of this shift is the recent investments by Elevance Health, Aetna, and Cigna in social supports ranging from nutrition, housing, and expanded mental health services.

One example of a major policy change—and innovative health plan programming in response—is happening in California. The Golden State is on the front end of a five-year overhaul of its Medicaid program, called Medi-Cal. The overhaul, CalAIM (California Advancing And Innovating Medi-Cal) has brought two new services, enhanced acre management (ECM) and community supports (CS), to the Medi-Cal Program.
In our August 18 Circle Elite Executive Roundtable, How California Health Plans Will Change Their Contracting Models & Network Management Under CalAIM, Rafael Gonzalez-Amezcua, M.D., Chief Medical Officer of Aetna Better Health of California, and Beau Hennemann, Regional Vice President of Local Engagement and Plan Performance for Anthem Blue Cross, described how their health plans are working with provider organizations to provide these new services to Medi-Cal members.
Aetna introduced ECM and CS as covered network benefits in its network—and have successfully transferred all of their eligible members to the new services. To do this, they have built a detailed reimbursement system, a customized platform for claims submission, and new procedures for utilization management.
“The health plan staff need to develop a better understanding of where CM’s responsibility ends and ECM begins and develop guidance re care management escalation trigger points”, said Dr. Gonzalez-Amezcua. “I think plan and provider leadership, in terms of expertise, knowledge, and authority to make changes, should know with mutual understanding what intervention is most appropriate and not just leave it to the staff to decide. This leads to more effective utilization of resources and improved health outcomes across the board.”
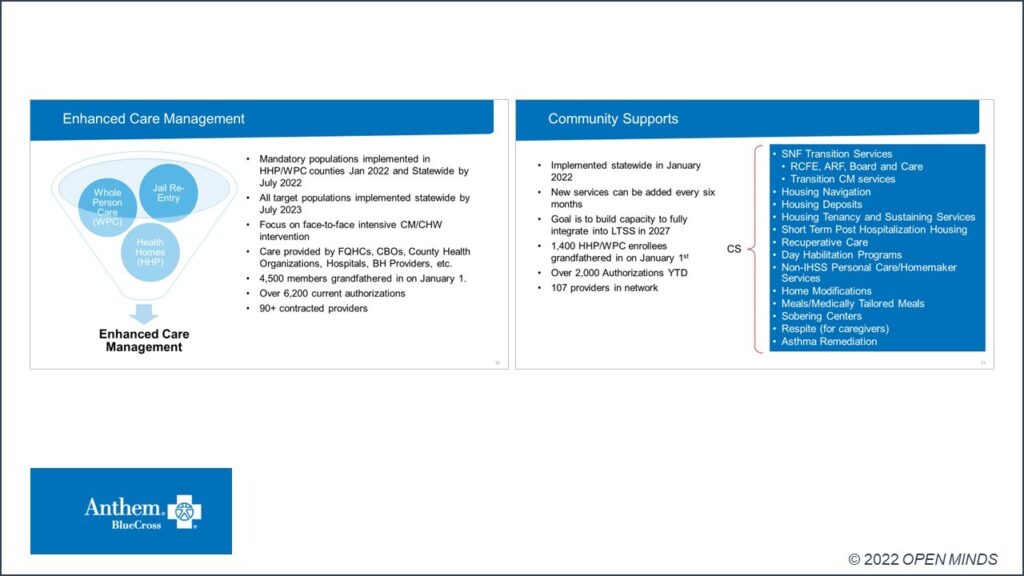
To facilitate this transition to new Medi-Cal member benefits, Anthem has developed a new provider certification process. The process includes an open letter of intent process and specific process for credentialing, contracting, and training. “It is important to build the initial infrastructure and capacity, and make sure that organizations coming on board have what they need to be successful in engaging consumers and connecting them to services,” said Mr. Hennemann.
This transition is not without its challenges for provider organization executive teams that want to participate in these new member service opportunities. There are contracting, credentialing, and data requirements. There are new processes for authorization and claims/billing. There are new reporting requirements.
And both executives mentioned the challenge in getting the medical community on board—particularly primary care professionals. “It is a false belief that it [addressing social determinants of health] is not useful,” said Dr. Gonzalez-Amezcua. “But I see it now that physicians do not want to be a part of it, but their buy-in and participation is important. We must articulate the benefits to primary care providers because if we address issues upstream on social determinants, mental health, etc., those are things that can help providers do their jobs more effectively.”
But those roadblocks are far outweighed by new service line opportunities for CalAIM provider organizations who are willing to build collaborative relationships with health plan managers. The key is to develop these new service lines with a solution-focused approach that meets both the needs of consumers and the fiscal and population health management goals of the health plans.

