The adoption of value-based care may be moving at a glacial pace, but it is growing. Just last week, Centene Corporation announced they are teaming up with Pearl Health, a technology firm, to improve how health care providers are paid by focusing on the value of care they provide, not just the quantity of services and Thyme Care launched a value-based care model focusing on cancer treatment.
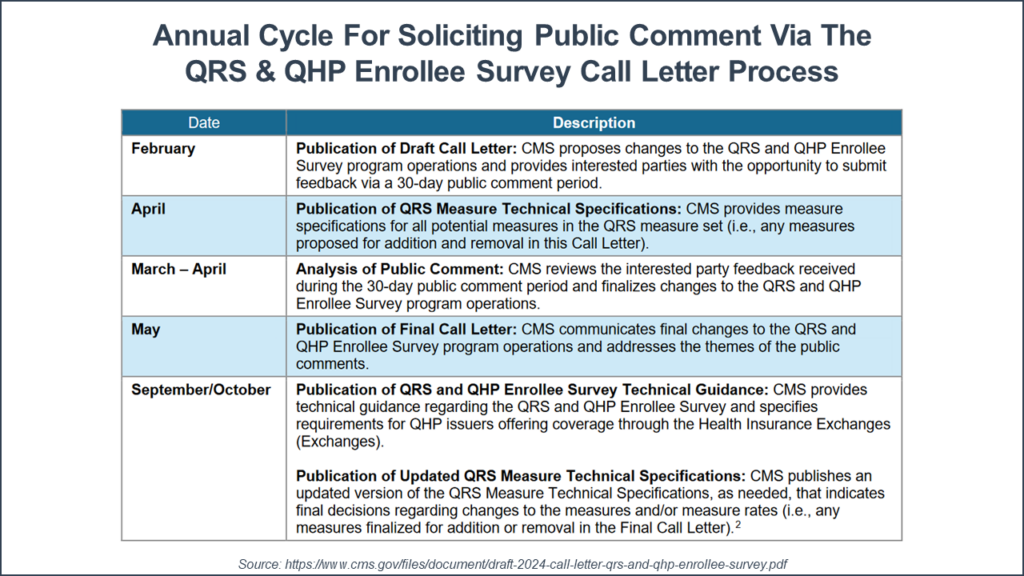
Fundamental to value-based care is the definition of ‘value’—and that definition continues to evolve and become more consumer-oriented. In February, CMS released a request for public comment (due by March 28, 2024) for possible revisions to the Quality Rating System (QRS) and Qualified Health Plan (QHP) enrollee experience survey for the Health Insurance Exchange (HIE).
The QRS rates the quality of health care services offered by health plans on the Health Insurance Exchange. Consumers can use the ratings to select a plan. Each year, CMS generates a report of all health insurance exchange quality rating systems. Guidelines and technical assistance for health plans and a full list of current QRS rating measures are available. And resources are also available to help consumers understand how to use these measures in their health plan choices.
There are a number of revisions proposed to the QRS/QHP measurement set. This includes the addition of two new measures and the discontinuation of one. And for some measures, CMS Is proposing to mandate the collection of stratified race and ethnicity data.
The first new measure is Social Need Screening & Intervention (SNS-E). This measure was developed by the National Committee for Quality Assurance (NCQA) to identify gaps in food security, housing, and transportation. The second measures Depression Screening & Follow-Up for Adolescents and Adults (DSF-E). This measure was adapted by NCQA from the provider measure “screening for depression and follow up plan”. This measure scores the rate of individuals (12 years and older) who received a clinical depression screening, scored positive, and received follow-up care.
Both measures were first proposed in 2023; however, due to public comments and concerns, including the Electronic Clinical Data Systems (ECDS) submission, they were not implemented for 2024. The ECDS is the data framework for health plans to report data from their EHR, case management, and/or administrative systems. If adopted, these new measures would apply starting with the 2025 ratings year with scoring inclusion starting the earliest in 2026. Both measures are collected through ECDS
One measure is slated for removal from the QRS. The antidepressant medication management (AMM) measure will be removed from the scoring criteria after 2025. NCQA is retiring this measure because it focuses solely on medication compliance. The proposed depression screening and follow-up measure would replace the AMM measure in the QRS set.
Additionally, four physical health measures and one behavioral health measure are being proposed for collection and stratification by race and ethnicity data starting in 2025. Beginning with the 2025 ratings year (i.e., 2024 measurement year), CMS proposes to expand the required collection and submission of stratified race and ethnicity data by QHP issuers for the following five measures: eye exam for patients with diabetes, follow-up after hospitalization for mental illness, kidney health evaluation for patients with diabetes, childhood immunization status, and cervical cancer screening.
The QRS system is important for organizations offering health plans on the health insurance exchange marketplace. Consumers use the ratings to select a plan. Health plans use a combination of provider, member, and claims data and advanced analytics to optimize their scores and develop interventions to increase QRS scores and improve health equity. These interventions may be specific to a group of individuals, geographical locations, or nationally.
My colleague, OPEN MINDS Senior Associate Margaret Mays, says, “With the two new risk stratification measures included in the QRS rating system, health plans will be able to identify health inequities and be required to produce effective interventions. By adding stratification to the ambulatory follow-up measure, interventions can be developed to address disparities and increase the rates.”
The health plan focus on QRS scores has a direct effect on provider organization executive teams looking to optimize their relationship (and revenue) from health plans. First and foremost, these are the ‘value’ factors that health plans are looking for in provider organizations in their network. Executive teams need to consider how best to measure and manage their performance on these factors. And when that performance is good, use that to negotiate better rates and preferred referral status from health plans.
The other factor is the infrastructure required to measure these performance metrics—and report them to the heath plans. Executive teams should evaluate the capacity of their system to calculate the data and submit it to their health plan partners. And the most important note, the definition of ‘value’ is likely to change over time—and any investment in systems need the flexibility to change.
Margaret Mays adds that “health plans’ increasing focus on clinical data exchange and health equity initiatives has made it imperative for provider organizations to take action and focus on three areas within their organizations to assist in improving QRS scores: deploy agile clinical systems, implement data sharing protocols and analysis, and implement change management processes to align the organization with health equity initiatives.”
Executives of specialty provider organizations are encouraged to evaluate their clinical and data systems for reporting and update policies, training, and programs to align with these new QRS measures. Investing in the clinical data systems and infrastructure required will enable organizations to modify and ensure their clinical workflows are aligned with new best practices and measurement standards.
