By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Consistency is a must in the current health and human landscape. It’s a by-product of the push for “value.” Consumers and health plans managers are looking for clinical programs that have consistent treatment plans, consumer experience, and results. With health plans controlling an increasing share of the market, provider organizations that can replicate a high-quality program have the market advantage.
In this market, which puts a premium on performance and scale, a focus on evidence-based and evidence-informed practices (EBP) is an asset. Using EBP, defined as clinical care informed by the best available science, to drive clinical program design and management provides valuable differentiation in a crowded market with the focus on performance—i.e., the EBP-based focus keeps clinical programming ahead of the curve. Since there is a 17-year “lag time” from research evidence to clinical practice, using EBP generally requires a structure in a clinical program that facilitates replication. But many provider organizations are missing out on this obvious strategic winner—only a fraction of clinical recommendations are evidence-based.
One organization is leveraging EBPs to gain market share, and this was the focus of the recent OPEN MINDS Executive Roundtable, From Evidence-Based Practice, To Pilot, To Outcomes: The Youth Advocate Programs Case Study. The session featured Gary Ivory, President and Chief Executive Officer, and Jennifer Drake, National Director of Behavioral Health Services, of Youth Advocate Programs (YAP), Inc. Their team collaborates with stakeholders in 35 states and the District of Columbia in the youth justice, child welfare, behavioral health, educational, and other systems delivering services that give communities alternatives to incarceration, residential placements, and neighborhood violence. A study by the John Jay College of Criminal Justice research of YAP’s wraparound services model found that 86% of YAP’s youth justice participants remain arrest-free, and 90% still live in their communities. Six months into the program, 90% of participants had no additional contact with the legal system.
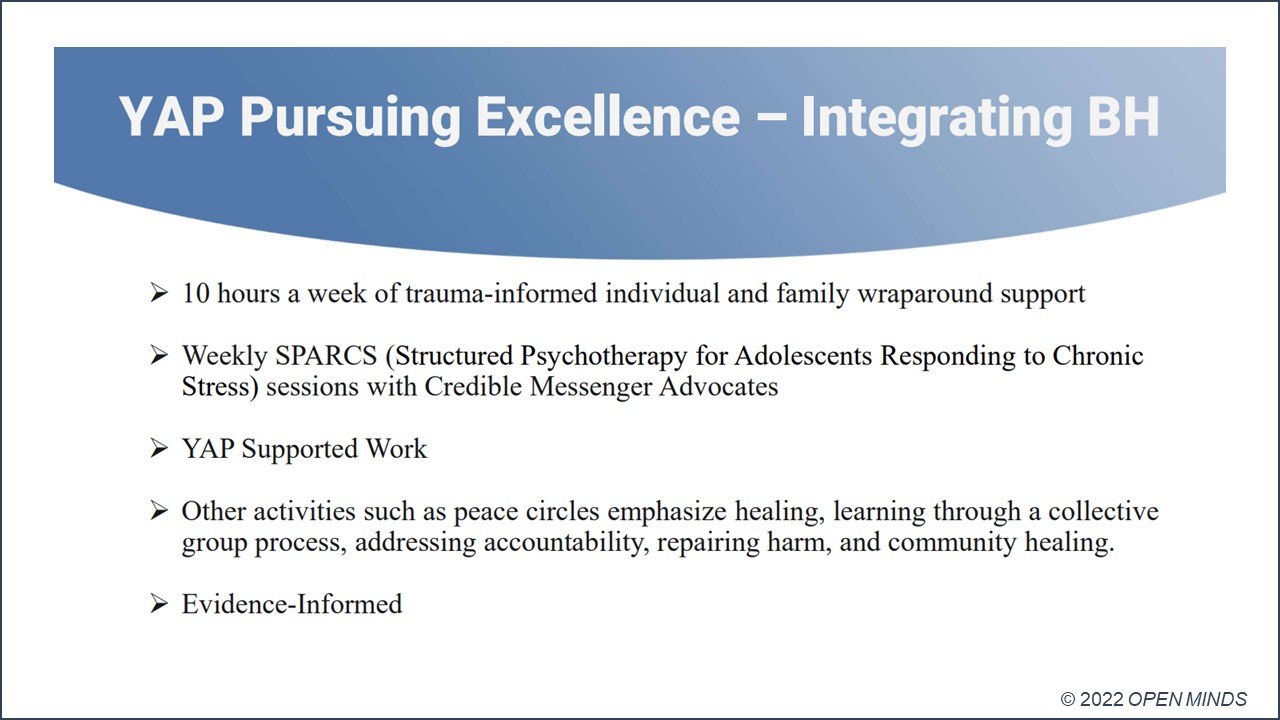
YAP has grown evidence-based and evidence-informed service lines over the past decade. As an example, the speakers presented the YAP Pursuing Excellence™ program—a violence reduction program that integrates behavioral health into YAP’s evidence-based youth and family wraparound services model. The violence prevention intervention youth ages 12 to 18 in five New Jersey counties, including those with a history of school suspensions, truancies, violent behavior, and/or those dealing with mental health or substance use issues. YAP launched the New Jersey Community-Based Violence Prevention Program in 2022 in partnership with The New Jersey Department of Community Affairs. The program model includes ten hours a week of trauma-informed individual and family wraparound support, along with weekly SPARCS (Structured Psychotherapy for Adolescents Responding to Chronic Stress) sessions for youth with the highest risk of gun violence. Some participants also have YAP Supported Work jobs, where local businesses provide work experience and the youth are compensated by the nonprofit.
YAP Pursuing Excellence™ is modeled after Choose to Change™ (C2C™), where YAP combines its evidence-based alternative-to-youth incarceration/residential placement youth and family wraparound services with weekly SPARCS sessions delivered by BrightPoint (previously Children’s Home & Aid).
The results have been impressive. Through a randomized controlled trial, researchers at the University of Chicago Crime Lab and Education Lab have found that C2C™ reduces violent-crime arrests by almost 50% and increases attendance in school by about a week.
Mr. Ivory and Ms. Drake also shared their ‘lessons learned’ in building a program based on EBPs—namely, using that program structure to drive growth. They emphasized three elements that executives should consider when bridging the gap between EBP as a good idea and EBP-informed success: continuous quality improvement, consumer monitoring, and a dedicated team.
Continuous quality improvement (CQI)—CQI is at the heart of any provider organization’s attempt to use data and is critical for using an EBP-based approach to growth. The key is to embrace “continuous” as part of regular performance reviews and operational adjustments.
“We are constantly looking at how we can improve quality,” said Mr. Ivory. “We look for early warning signs showing if programming is not trending right, so we can intervene quickly and make sure we’re on target. Outcomes are very, very important.”
Consumer monitoring—EBP isn’t strictly “all about the numbers.” A great clinical service line with poor consumer experience will miss the strategic mark. That leads to poor consumer experiences. And poor consumer experiences will decrease service line participation and performance.
“We have three levels of consumer monitoring,” said Mr. Ivory. “We have phone monitoring where we call every family every month and ask if they are satisfied. We send letters to families, as well. And then our program directors have direct contact with the family. So we do a lot of monitoring and quality assurance. We think that’s all part of running a high-quality program.”
A dedicated team—Meaningful EBP adoption, deployment, and use monitoring require a dedicated team that can build and run the infrastructure to fully realize the clinical, quality, administrative, and financial requirements. A big part of this will include training your clinical professionals in the different EBPs.
“We work very closely with our employee and program development teams,” said Mr. Ivory. “They offer a blend of recorded self-learning and in-person learning. We also invested in a system because our staff wanted access to continuing education. And our leadership in each state knows what the training requirements are, and they work with our training team to make sure that’s available in all formats.”
Standardization of services around evidence-based best practices is an increasingly essential attribute of competitive success. The challenge for most provider organization executive teams isn’t the technology or the clinical models. The challenge is a shift in culture—with a focus on data-driven decision making in clinical service line development and growth strategies.
