By Monica E. Oss, Chief Executive Officer, OPEN MINDS
When it comes to whole person care models, the question is—what’s working? According to the report, Community Supports, Or In Lieu Of Services (ILOS), Annual Report, on California’s Medicaid reform initiative—California Advancing and Innovating Medi-Cal (CalAIM)—the uptake and outcomes of their community supports programs are impressive.
Under the CalAIM initiative, the Medi-Cal managed care plans (MCPs) have operationalized a menu of fourteen (14) community supports benefits. Twelve (12) are state-approved In Lieu of Services (ILOS) benefits, and two are authorized under the Section 1115 demonstration (an in lieu of service or setting—ILOS—is a service or setting that is provided as a substitute for a covered service under the plan, when the substitute service can be expected to reduce or prevent the future need of a service).
The new data—from Q4 2023 to Q3 2024—shows there were 95,143 unique users of the community supports services in that time period. Medically-tailored meals had the highest utilization, followed by housing-related community supports—including housing transition navigation services, housing deposits, and housing tenancy and sustaining services.
With regard to cost-benefit, nine of the community supports have already been determined to be cost-effective—housing transition navigation services, housing deposits, respite care, day habilitation programs, nursing facility transition/diversion to assisted living facilities, community transition services/nursing facility transition to a home, personal care and homemaker services, environmental accessibility adaptations, and sobering centers. Three remaining ILOS—housing tenancy and sustaining services, medically tailored meals, and asthma remediation—have demonstrated reductions in service utilization and per member per month (pmpm) spend.

The community supports with the greatest impact on net pmpm costs include housing deposits (−31.6%); day habilitation programs (−17.1%); transitional supports from a nursing facility to an assisted living (−30.3%); community transition services/nursing facility transition to home (−21.5%); environmental accessibility adaptations (−14.5%); and sobering centers (−11.7%). These early results speak to the cost-effectiveness of whole-person care models and the reimbursement for meeting consumer health-related social needs.
We got an in-depth look at two models for making whole person care work in California in the session The Next Generation Of Integrated Care: Making It Work With Catholic Charities of Santa Clara County & The Children’s Institute at The 2025 OPEN MINDS Service Excellence Institute. The executives leading the session—Monica Dedhia, Director of Community Health, Children’s Institute, and Don Taylor, Chief Executive Officer, Catholic Charities of Santa Clara County (CCSCC)—presented two innovative models for meeting the needs of consumers with health-related social needs.
Headquartered in Los Angeles, the Children’s Institute is a $111 million provider organization serving children and families impacted by trauma and poverty. Its core services include behavioral health, wellness, early childhood education, and community health. Serving over 30,000 children and families annually across LA, the organization has been at the forefront of California’s CalAIM reforms by advancing community supports. CCSCC, headquartered in San Jose, California, is a $57 million provider organization that is the social service and social justice arm of the Catholic Diocese of San José. It works to alleviate conditions of chronic poverty by providing food, housing assistance, access to benefits, senior services, and mental health services. It serves over 119,000 people annually across more than 85 locations in Santa Clara County, employs over 500 staff members, and engages more than 1,600 volunteers.
The Children’s Institute faced three converging strategic challenges—the CalAIM mandate to operationalize whole person care across Medicaid populations, addressing historical inequities in underserved communities, and creating, building, and managing the partnerships necessary to support cross-sector collaboration. In response, they implemented CalAIM-associated community supports and launched the Watts Community Wellness Initiative. The door-to-door engagement model provides a “navigator” to help residents access services across multiple systems, perform household visits and assessments to capture social needs, and link consumers to preventive supports, including direct scheduling of primary care visits, screenings, and assistance with managing Medi-Cal benefits.
The Children’s Institute initiative was successful in advancing whole person care through improving access. Their program conducted 8,000 household visits in Watts by community health workers, completed 100 primary care appointments through direct scheduling, provided preventive screenings to 163 families, and connected 26 families to Medi-Cal coverage.
CCSCC was challenged to address rising poverty, housing instability, immigration-related disruptions, and deep inequities in behavioral health access in the communities it serves. Heavy reliance on government contracts—representing 65% of revenue—added financial and operational volatility to its prospects for long-term financial sustainability.
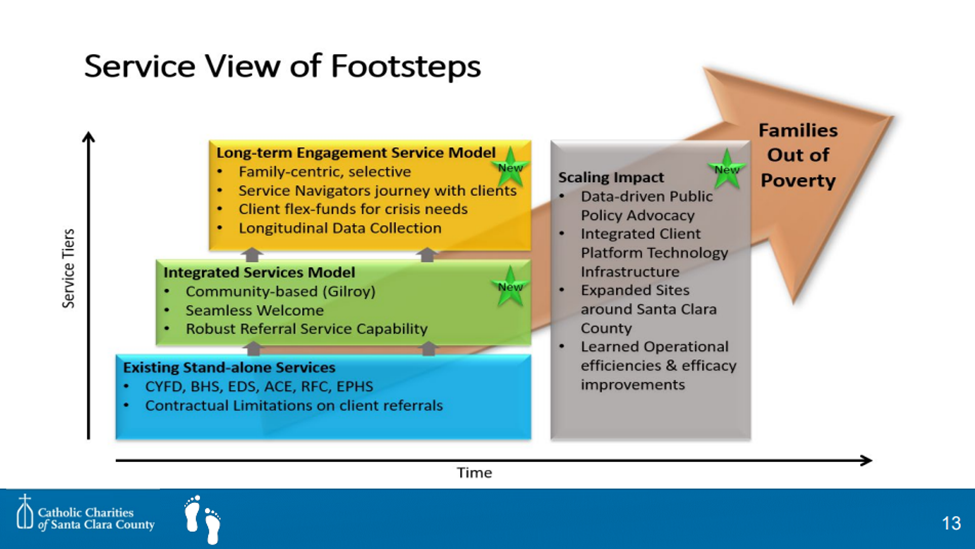
To meet these challenges, CCSCC launched “Catholic Charities’ Footsteps”—a family-centered community change initiative to disrupt poverty. Strategically implemented as its integrated care approach, the initiative is designed to move beyond episodic service delivery toward long-term, side-by-side engagement with families. Its “no wrong door” approach offers consumers multiple entry points to a range of services and supports.
The outcomes for this approach included tripled engagement in target neighborhoods and increased cross-program utilization within CCSCC’s service portfolio. Highlights from one South County Neighborhood showed enrollment in the program grew from 327 families in 2021-2022 to 2,787 families in 2024-2025. And CCSCC maintained 60% of its public funding level despite public funding cuts, increased private funding, and increased strategic reinvestment by 60% to support its financial sustainability.
To initiate, support, and expand whole person care initiatives, the speakers spoke to three areas of focus for successful whole person approaches focused on consumers and families with social support needs. These include increasing long-term consumer engagement, extending cross-sector collaborations, and executing data-driven equity strategies.
Both executives emphasized that episodic, short-term service encounters don’t change health trajectories in the same way long-term consumer engagement can. Training programs that teach all staff to see “every door as the right door” and enable consumer connections to community supports for housing, food, legal services, health care, and behavioral health services can make a difference for the future. This approach may involve redefining what success means. Service units delivered is still an important measure, but “journey outcomes” such as stability, resilience, and reduced poverty are the end goal of whole person care tied to community engagement.
“We work with a family side by side to help understand their needs and help them access and receive services,” said Mr. Taylor. “In their journey, they become increasingly stable and sufficient. It’s a long-term perspective.”
Strategic partnership was another key to a broad-ranging approach to whole person models of care emphasized by the speakers. It is not possible for most organizations to provide all services that a group of consumers may need. An effective system requires leaders to structure their teams to stitch together an extended network of provider organizations and community services organizations to meet consumer needs for housing, food, education, immigration support, behavioral health services, and other health care services.
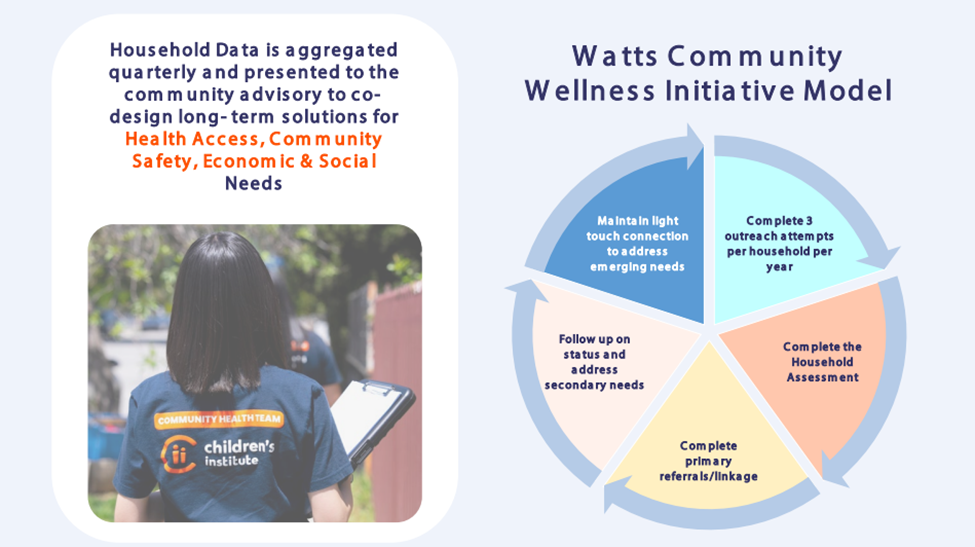
“We are mobilizing partners so that we can be more cohesive in our response rather than siloed,” said Ms. Dedhia. “We experience a lot of folks doing a lot of good work, but doing it very separately or in a duplicative manner. The question is, how can we utilize the data that we are bringing in to mobilize partnerships in a more cohesive and fundamental way that will meet needs?”
And finally, a data-driven equity strategy is essential. By quantifying community needs through data collection and analysis, executives can make an evidence-supported case for integrating non-medical supports while creating urgency and credibility with payers. Executives should prepare to collect data and provide analysis that is actionable to show where poverty, race, and geography intersect with health, and then build their solutions using those data points. That structure can support both advocating for systemic funding changes and tracking success.
“Look at the data from a systems change and policy advocacy standpoint,” said Ms. Dedhia. “How are we integrating this data into our policy agenda so that when we’re in various spaces or using partners, we lift the priorities of our communities? How do we engage local governments? There is value-based reimbursement in the data that we’re collecting. Can we pitch this to a performance-based type of pay where we are looking at those sustainable outcomes?”
For executive teams of traditional specialty care provider organizations, moving to whole person care models will be a challenge. Mr. Taylor noted that success is a matter of aligning overall organizational strategy with the budgets and operations of individual programs. He said they have used change management approaches to support a whole person care oriented culture going forward. “We regularly visit the teams…and give them more organizational updates…tying staff outcomes to the broader outcomes. When individual programs connect to successes with our initiative, we’re celebrating them.”
