A few weeks ago, the Institute for Exceptional Care (IEC), released the National Roadmap For Disability-Inclusive Healthcare. The focus of the roadmap is to improve health care for consumers with intellectual and developmental disabilities (I/DD) by giving clinicians the skills to care for these consumers.
Not surprisingly, people with disabilities are more likely than the general population to have unmet health care needs, receive lower quality health care, and fewer preventative services—with 25% of adults with a disability not having a primary care professional and 20% not having a routine checkup within the past year. Clinicians are not prepared to serve the population with disabilities, with only 57% of physicians agreeing that they “welcomed people with disabilities into their practices”. This is not surprising since medical students receive an average of 11 minutes of exposure to I/DD throughout their four-year clinical training.
In addition, health care for consumers with I/DD suffers from a lack of coordination between programs for primary and behavioral health care, acute care, and home and community-based services. One policy initiative to bridge that care coordination gap is moving to managed care models for the financing and delivery of services. As of 2020, 22 states were operating 26 Medicaid-managed long-term services and supports (MLTSS) programs. Only ten states (i.e., Arizona, Arkansas, California, Iowa, Kansas, Michigan, North Carolina, Tennessee, Vermont, and Wisconsin) include I/DD consumers in those initiatives.
The question is how best to ensure that these managed care models work for consumers with I/DD. That was the focus of the session, Models Of Reimbursement & Payment For I/DD Service Delivery, at the 2023 OPEN MINDS I/DD Executive Summit. In the session, Marco Damiani, Chief Executive Officer of AHRC New York City, and Scott Doolan, Assistant Vice President of Health Care Management of Partners Health Plan, discussed the opportunities and challenges of managed care for the I/DD population for both consumers and provider organizations.
Partners Health Plan (PHP) is a non-profit demonstration project funded in a ‘three-way” contract by Centers for Medicare & Medicaid Services, the New York State Department of Health, and the New York State Office of People with Developmental Disabilities—a fully integrated managed care organization exclusively serving individuals with I/DD. PHP is essentially at full risk for consumer services as a health plan.
AHRC New York City supports 15,000 individuals with I/DD and their families. The AHRC NYC Crisis Transition Program is funded using a global budget arrangement. The model was initially funded by the New York City Health + Hospitals Corporation and the Mother Cabrini Foundation. It is now funded through the New York State Office of Mental Health. The transition program model is a clinical residential program for up to five individuals with IDD who experienced long-term inpatient stays.
The performance of the Partners model has been encouraging, reporting a 12% percent decline in emergency department utilization and 39% decline in inpatient hospital admissions. PHP members had more breast and colorectal screenings and more dental and primary care visits. And the PHP plan outperformed the national average in 7 of 8 Healthcare Effectiveness and Data Information Set (HEDIS) measures from 2019 to 2021. At AHRC, during its five years of operation, nearly 70% of referred consumers are served in a long-term community living arrangement—accruing substantial savings in payment for institutional care.
To make managed care models work for consumers with I/DD, the executives had three recommendations for health plan and provider organization executives—consumer assessments for population health planning; targeted interventions for the consumer population; and whole person care coordination models.
Consumer assessments for population health planning A critical element in making managed care models work for consumers with I/DD is gathering baseline data on consumers including known health risks like diabetes, high blood pressure, cancer, and vision and hearing impairments. This assessment data is used to create individualized prospective care planning and population-wide performance improvement initiatives. The PHP model involves a population-tailored I/DD-focused person-centered assessment and Life Plan framework that supports health promotion and delivers a person-centered plan of rehabilitative interventions for functional, medical, behavioral, and social concerns.
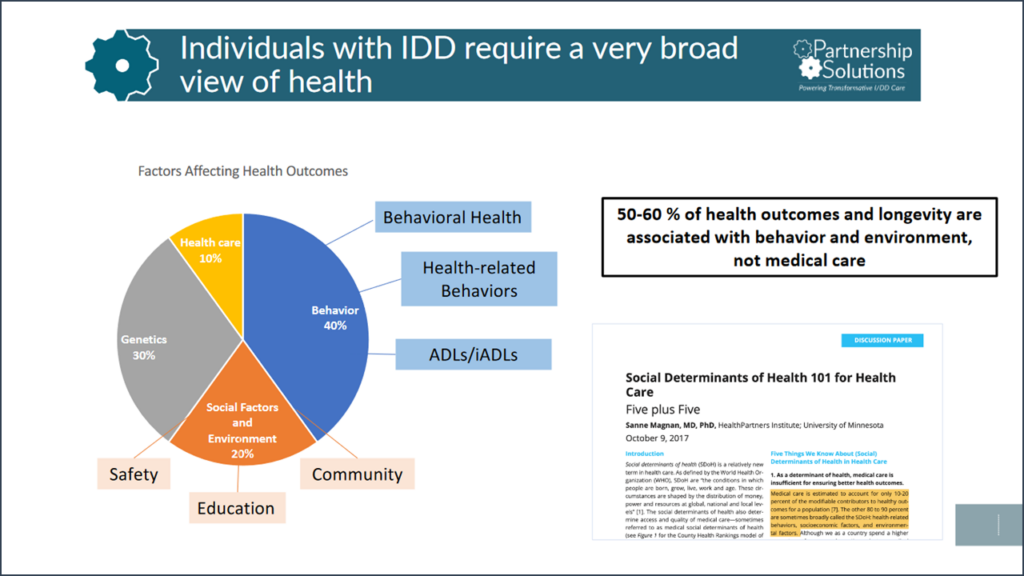
Targeted interventions for the consumer population Using the assessment data as the baseline, another key element in the successful application of managed care models for the I/DD population is creating care plans that are specific and person-centered. This approach to care management is focused on preventive primary and dental care with a schedule of visits and follow-up care based on consumer health need complexity. Tracking consumer multi-drug regimens and medication adherence is key to planning interventions.
“Whole person” care coordination models The successful person-center model needs to use ‘whole person’ approaches to care coordination and health management. But this approach is difficult in systems that remain tied to fee-for-service reimbursement. Without the flexibility to fund active care coordination.
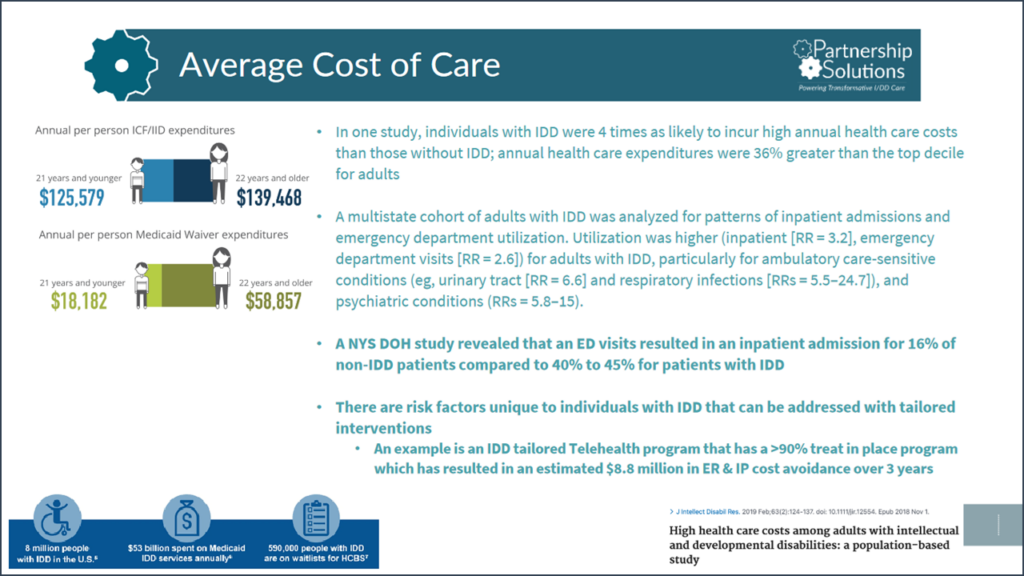
PHP used its payment flexibility to develop successful telehealth services within group homes, an excluded service under most health plans. Mr. Doolan explained, “To put some numbers behind it … the telehealth program… over three years, has an estimated $8.8 million in savings. If you push that out to the entire I/DD population of New York State, you’re looking at $56 million in savings at a very conservative level, which is likely much, much higher than that. So, it’s really that flexibility that we talked about needing to be able to move things around and put programs in place that truly work for the population and are designed for the population.”
Mr. Damiani emphasized that the right model leads to better results for consumers with I/DD. “They’re finally seeing that there’s this interstitial space and I/DD supports and services that are hurting people. And providers don’t want to enter that space. So, value-based payments, integrated care models, ways of incentivizing providers to take on these challenges are essential to giving people the life that they deserve to have.” Mr. Doolan agreed, “You need a system of payment that understands a lifelong set of needs and opportunities. Plans pay for sick people; they don’t pay for opportunities. And that’s an important thing to say a different way… we’re looking at supporting somebody in a way that gives them the life that they choose. “
