The new Kaiser Family Foundation (KFF) report on Medicaid Waivers Medicaid Waiver Tracker: Approved And Pending Section 1115 Waivers By State, is just out. And it confirms our news coverage over the past year—more states are adding housing benefits and other social services to their list of paid Medicaid services. There are now 18 states with approved housing support waivers. And 17 pending waivers adding some type of social support service (housing, nutrition, employment, etc.) to their Medicaid programs.
The shift in state waiver applications (and approvals) is attributed to the change from the Trump Administration to the Biden Administration. The current administration is focused on waivers that expand rather than restrict Medicaid coverage with an emphasis on reducing health disparities and/or advance whole person care, including addressing health-related social needs. (Though it is important to note that budget neutrality is still required.) And the Biden Administration has withdrawn approval of work requirements and is phasing out premium requirements in the Medicaid program.
Like everything about the Medicaid program, there are wide variations by state. Montana, Massachusetts, and Oregon have initiatives focused on housing.
New York and New Jersey have submitted waiver requests for broader social support initiatives. Both waivers were just approved, with some modifications, by Centers for Medicare & Medicaid Services (CMS).
There are a host of waiver requests still pending approval. In Pennsylvania, there is a current Medicaid 1115 waiver for Medicaid reimbursement for a new program, “Bridges to Success: Keystones of Health for Pennsylvania” (Keystones of Health), that will offer targeted supports and services. Hawaii is requesting payment for new programs focused on whole person care. And Illinois has submitted a request to extend its current waiver adding housing and community reintegration services for justice-involved adults and youths.
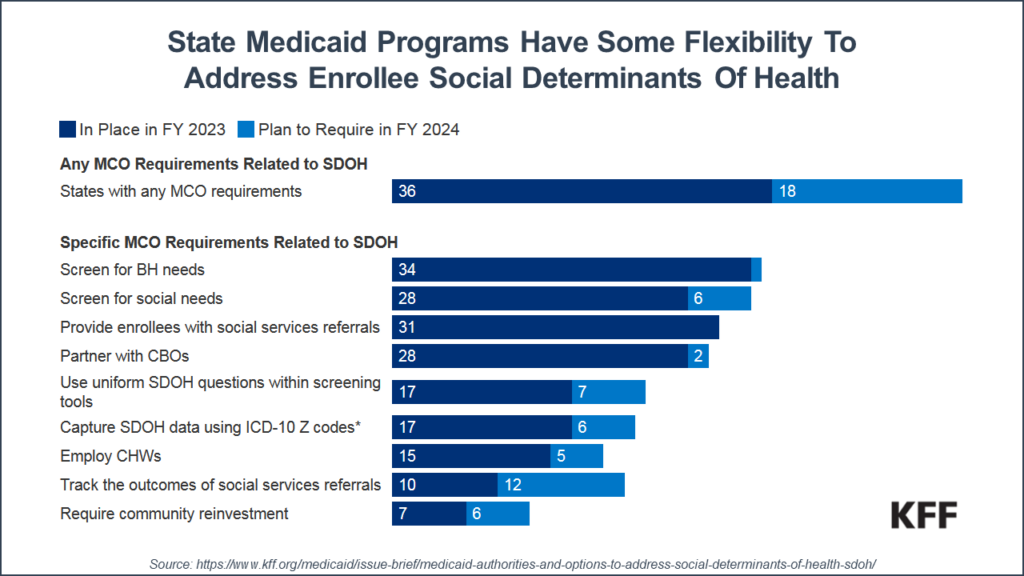
Not surprisingly, since 70% of Medicaid beneficiaries are now enrolled in some type of Medicaid health plan, those Medicaid plans have been given the flexibility to pay for non-medical services through “in-lieu-of” authority or as “value-added” services (that cannot be built into the Medicaid rates). In fact, most states now have some requirements related to social determinants for their Medicaid health plans. Most common are requirements to provide and pay for behavioral health and/or social needs screening, followed by requirements for social service referrals.
The implications for traditional provider organizations are many. For the 10% of U.S. health care consumers who use 70% of health resources, over half have a behavioral health disorder and even more are in need of some type of social support that will likely reduce their total health care spend. For those high-needs consumers, spending will start to shift to programs that incorporate whole person approaches integrating medical, behavioral, and social support needs. But it is not a matter of just offering more services. Managers of Medicaid plans and health plans are going to look for provider organization program offerings that have measurable outcomes, a measurable ROI, and some type of performance-based reimbursement. And with more Medicaid funding on the line (up to 5% of Medicaid health plan medical loss ratio), expect to see more competition for this new funding.
