By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Consumer experience with the health care system remains poor. 73% of consumers believe the health care system isn’t meeting their needs, 66% complain about rushed care, 49% express frustration with clinical professionals’ lack of understanding or listening, and 54% express a desire for provider organizations to assist them in navigating the system (see Dedicate Your Organization To Improving Consumer Experience). And we know that even the lowest expectations aren’t being met. 46% of consumers cite service delivery problems as a key issue, 45% cite communication problems, and 39% cite negative employee interactions as the major issue (see The Consumer Experience Puzzle). For a competitive edge, health care provider organizations need a better consumer experience—from first call/website inquiry through service delivery to post-system wellness/disease state management.
To solve the problem, health care organizations are spending a lot on technology—particularly CRM systems, electronic health records (EHRs), and icare coordination platforms. The CRM market alone in health is projected to reach $37.62 billion by 2030 (see Healthcare CRM Market- Registering a CAGR of 14.1% By 2030).
But the increase in investments hasn’t yielded a measurable improvement in consumer experience. There seem to be two factors. The first factor is that the consumer experience in the health care system is more than the traditional retail consumer experience. A consumer’s overall health care experience consists of three parts. The first part is the consumer’s purchasing experience—where consumers evaluate services like any retail customer. The second part is the clinical experience, which is about quality of care and ease of navigating service delivery. The third part is the wellness and disease management experience, which is about quality of life after discharge (see CRM: The Wrong Acronym For Healthcare).
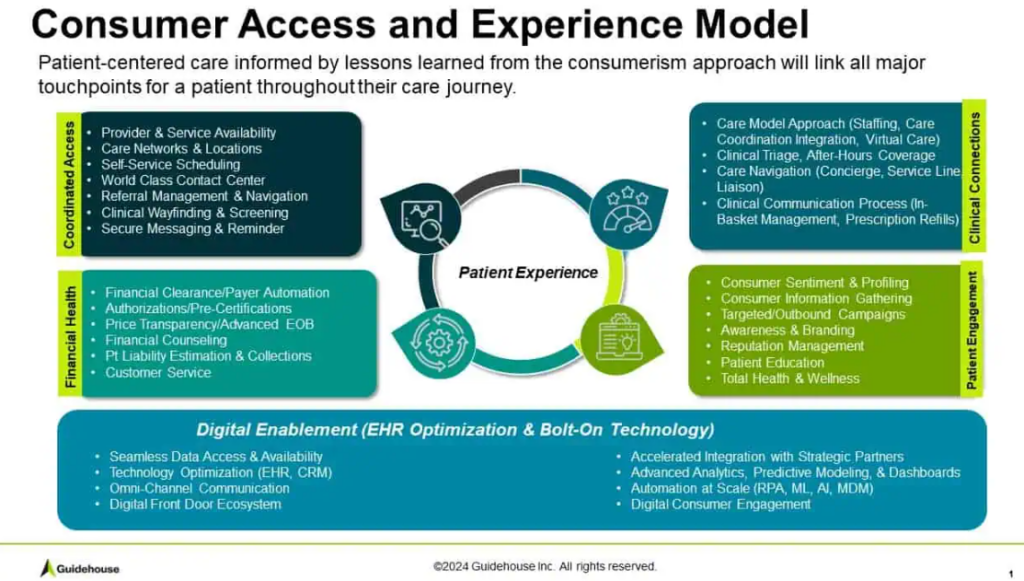
Currently, in most health care provider organizations, these three functions are ‘owned’ by different parts of the organization—and different team members in the organization. And different technologies support each of these operations.
CRM systems bring contact information, initial inquiries, scheduling, and other traditional retail functions to the purchasing experience. The EHR systems support the clinical experience. But they were designed primarily as billing systems—with their clinical information secondary to financial records and the ability to create reimbursable claims. Finally, the post-service care coordination functionality is just that—the longitudinal planning and outreach based on consumers’ clinical records and medical, behavioral, and social assessment data. The technological and systems problem is that most of the consumers’ data and qualitative contextual information gained along the way is lost from one step to the next.
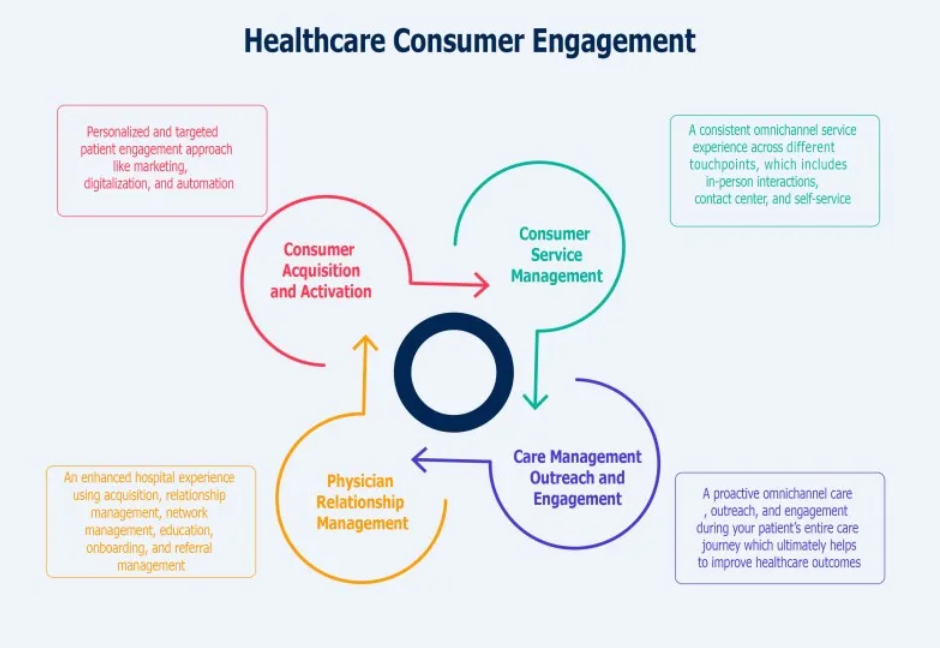
But the challenges of three separate management functions with three separate technology platforms create challenges, that situation isn’t the primary problem in improving consumer experience. Investing in the technology alone won’t transform the consumer experience. Health and human service executive teams need to reengineer the consumer journey and clinician workflows—and create an integrated set of performance measurements and team incentives that prioritize consumer experience.
With the current dismal performance in the health and human services field, there is an opportunity for competitive market advantage for provider organizations with even minimal efforts to improve consumer experience. And as the field moves to more whole person care models and value-based reimbursement, better consumer experience is the key to better consumer engagement—which has been demonstrated to improve health outcomes and reduce overall costs (see VBR For Equity).
In a recent interview, my colleague Diane Hopkins, author of two books on consumer experience—Advice from a Patient and Unleashing the Chief Moment Officers: Reliably Giving the Gift of Exceptional Experiences—observed, “It’s important to elevate consumer and employee experience as a strategic priority. A commitment to building internal expertise to design and sustain exceptional experiences is an investment that supports quality, market differentiation, staff retention, and customer satisfaction. And technology turned on does not solve consumer or staff issues. There must be a deliberate and thoughtful plan in place to blend technology-enabled enhancements with clear needs and preferences of consumers and staff.”
She went on to say, “For those just beginning to develop a consumer experience strategy, the first step is to pursue an honest assessment of the current state. It’s important to identify how staff are prepared, how operations are designed to exceed consumer expectations, and how feedback is collected and shared in order to create exceptional experiences. It’s also important to align leader and staff performance reviews to consumer satisfaction and to begin consistent work to strengthen the culture around consumer centric thinking.”
For executive teams that want to excel at consumer experience, certainly investing in the technology components of a digital platform for consumers and team members is essential. But making that investment pay off requires starting at the end. Start by measuring the key metrics of consumer experience—access times, no-show rates, return visits, and net promoter scores. These metrics become the baseline for moving a clinical organization from one that consumers “have to go to” to one they choose.
