By Monica E. Oss, Chief Executive Officer, OPEN MINDS
I think we’re in the post-pandemic doldrums. So many parts of the economy seem to be operating “not quite on par”—the airlines, our educational institutions, and our health care system to name a few. So, it was refreshing to learn more about a plan to find and reward ‘excellence’ in behavioral health in the keynote presentation at The 2022 OPEN MINDS Strategy & Innovation Institute, Filling In the Gaps: How Evernorth Is Driving Better Health For Complex Consumers, by Douglas Nemecek, M.D., Chief Medical Officer for Behavioral Health at Evernorth.
Dr. Nemecek described the four key elements of excellence in behavioral health systems—consumer access, consumer navigation, managing high-cost complex care, and integrated care delivery, as well as Evernorth’s approach to improving each of those domains.

Consumer access—Timely consumer access to behavioral health services is one of the key problems in the delivery system. Many consumers choose to use the emergency room when primary care isn’t immediately available, and lack of timely access has been linked to higher total health care spending. Evernorth has prioritized access to care as a key feature of a high-quality behavioral health system and their approach includes using digital tools and digital delivery systems to make access faster and easier.
“The first building block is access, how do we get people to care, and how do we do it quickly?” said Dr. Nemecek. “How do we make sure that people can do it simply, easily, and quickly. We’re measuring how long it takes to get someone into care and working with provider organizations to who can provide access to care more quickly, and reimbursing accordingly. That’s important to the individual, to whoever is paying for the care, and important for getting them engaged.”
Consumer navigation—Consumer choice is great, but in a complicated health care system it can also be confusing. Providing consumers with the information and the tools to make the right choices about their care is key to improving both consumer experience and consumer outcomes.
“This is a big one for us as we figure out how to help people understand where to go and make that connection,” said Dr. Nemecek. “How do we share information to get them scheduled for appointments in an easier and simpler way, instead of making them call around town trying to find someone, or going on Google trying to figure out how this works? By giving them direction on the resources with the right intensity of care from the very beginning.”

Managing high-cost complex care—For consumers with long-term, complex behavioral and medical conditions, enhanced tools and services are essential to ensuring better consumer outcomes. While that population is small (less than 10% of the population) the resource needs of these consumers are high and are often not well served by the tools designed for most consumers. To that end, Evernorth has developed an enhanced care coordination program that is fueled by integrated data, augmented intelligence, and predictive risk identification.
“The key here is, there is not one single point solution that can fix this for everybody,” said Dr. Nemecek. “We can’t forget about those consumers with severe and persistent mental illness. As a payer we must ask providers what population are you really good at serving, and how do we partner on that population? How do we say, who are the good providers, what are the demographics of those populations, and how do we do that across the full spectrum of needs? As a plan we need to do that for everybody, and we need multiple partners to help us meet those needs.”
Integrated care delivery—Last but not least, behavioral health services need to be part of an integrated approach to addressing consumer needs. The approach to care planning at Evernorth includes integrated data for care coordination across medical, prescription and specialty drugs, clinical, behavioral health, biometrics, telephonic and call data, and social determinants of health.
“How are we coordinating this in a holistic way?” asked Dr. Nemecek. “How are we connecting all of these pieces together so that we are optimizing the outcome, optimizing the health of the individual, and optimizing the affordability as well. One of the things we are doing is looking at how to expand that network, and those providers.”
To make these four key elements of behavioral health treatment excellence a reality on the ground, Evernorth has rolled out their center of excellence model. The results are impressive—costing 84% less with 37% lower readmission rates. For substance abuse treatment, centers of excellence cost 240% less and have a 71% lower re-admittance rate.
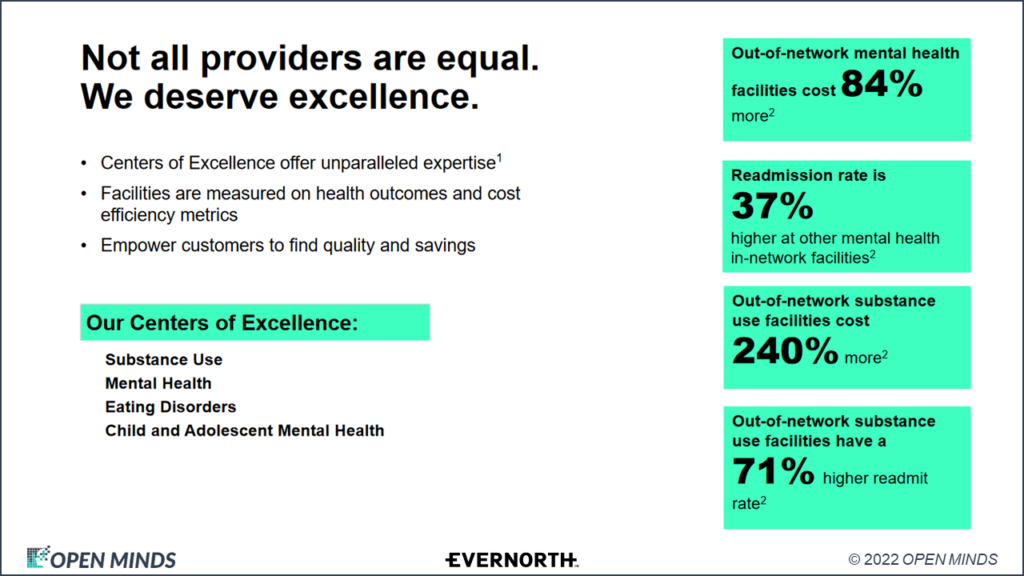
“How do we start to designate centers of excellence?” said Dr. Nemecek. “We started with substance use disorders and now have mental health facilities for both adults and adolescents, and eating disorder facilities that we consider centers of excellence across the country as well.” He also noted that they are looking for provider organizations with facility-based services who are part of the broader Cigna provider network—and have both an identified niche and demonstrated performance metrics for their programs.
Dr. Nemecek made an observation that stuck with me—”From a mental health standpoint, we are getting more into specialties,” he said. “If you think about it using an orthopedic example, none of us go to a generalist, we all go to a knee specialist, the hip specialist, the back specialist. With mental health and substance use, we are starting to see that.”
For executive teams who are looking to move their relationships with health plans to partnerships based on value, these centers of excellence initiatives are one of many approaches. The key is to focus on the core elements of being a great partner—targeted consumer groups and treatment protocols, documenting clinical program costs, and collecting outcome and performance data.
