By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Our last OPEN MINDS national survey found that 42% of specialty provider organizations had one or more payer contracts that paid them a ‘bonus’ based on performance. The question we didn’t ask is what percentage of those organizations actually got paid that bonus.
In our work with provider organizations around performance-based and value-based reimbursement models, there are two important factors in making performance-based incentive plans work. The first is having data needed for the contract negotiation process—knowing how your organization’s current performance on those metrics and the overall experience of the health plan on the measures. The second is having the ability to measure organizational performance on each metric on a relatively real time basis—and to manage that performance.
But how do executive teams build the analytic capabilities to maximize performance-based payments? And how do they make them sync with their current EHRs systems? Those questions were the focus of the case study presented in the session called Technology Tools For Improving The Performance Of Value-Based Contracts during the 2023 OPEN MINDS Technology & Analytics Institute. Rachelle Glavin, Senior Vice President Strategic Initiatives at the Missouri Behavioral Health Council (MBHC) and Tom Petrizzo, Chief Executive Officer of Beacon Mental Health, presented a case study of one of the longest-running value-based reimbursement arrangements for behavioral health provider organizations in the country—the Missouri Medicaid integrated care initiative.
MBHC is the organization representing 33 behavioral health provider organizations in Missouri. Their team develops programs and promotes behavioral health best practices across the state. Beacon Mental Health, formerly Tri-County Behavioral Health Services, is an MBHC member providing behavioral health services for children and youth in Missouri’s Clay, Platte, and Ray Counties. Beacon has 190 staff members and an annual budget of $30 million.
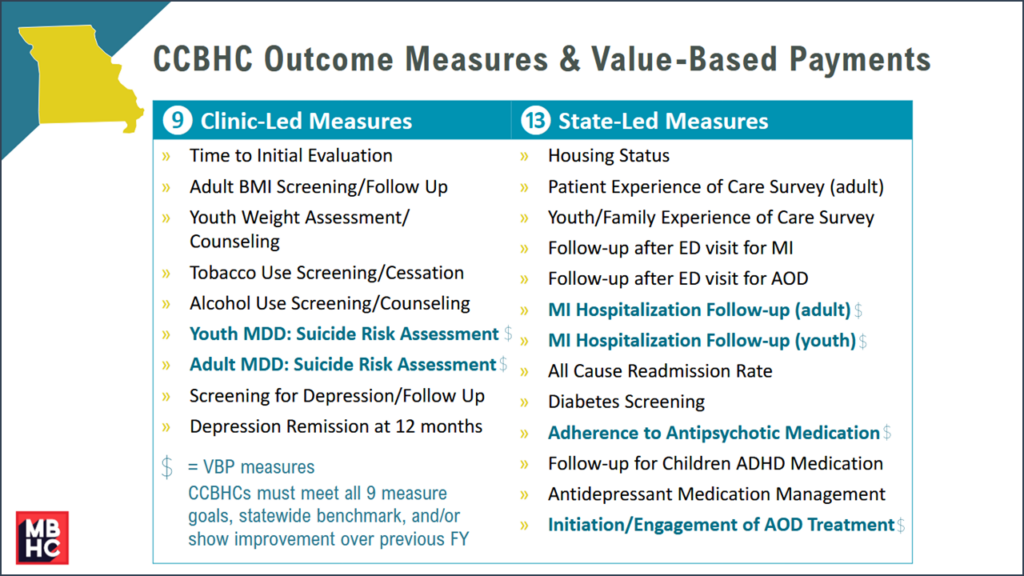
The Missouri Medicaid integrated care initiative started in 2008—with a focus on integrating physical health services into the behavioral health delivery system for consumers with multiple chronic conditions, including serious mental illness. By 2012, Missouri Medicaid had 26 behavioral health homes in operations. The program evolved into 15 (and now 20) Certified Community Behavioral Health Clinics (CCBHCs).
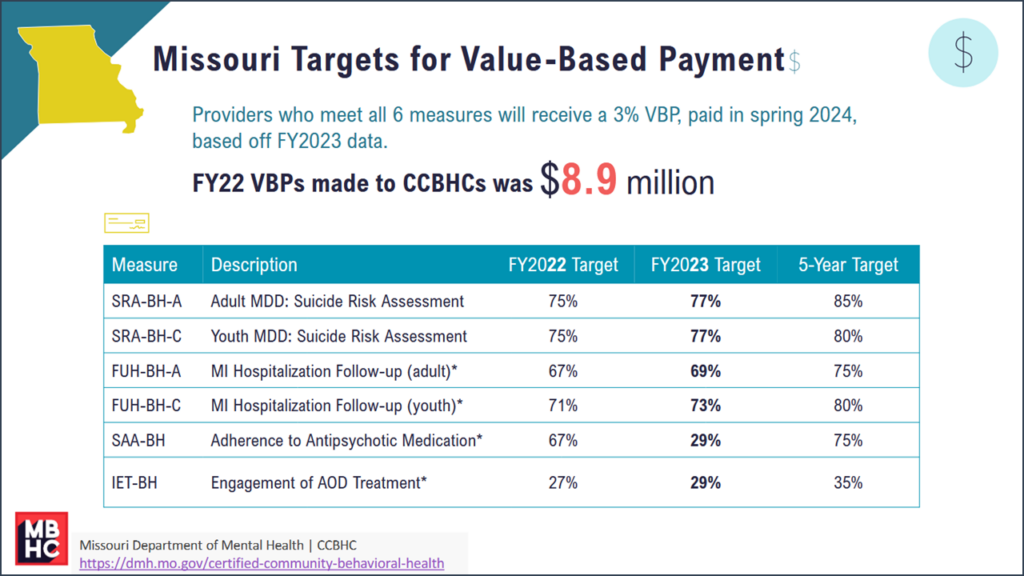
The Missouri behavioral health provider organizations have succeeded in hitting the system performance objectives and earning their performance-based bonuses—$8.9 million in 2022. The advice of the presenters to the audience was to think “one-stop shop”—one consolidated data set and one platform for data reporting performance data on a daily basis. They identified a few keys to creating this one-stop performance reporting initiative—interoperability and the elimination of double entry of clinical data; custom reporting in aggregate, at the clinician level, and at the consumer level; access to near real-time data; and automated risk stratification that displays in a way that enables population health management by care teams.
The most critical element in a system for performance management is creating a single data set of all data relevant to the consumer and the population. In Missouri, MBHC created an initiative that combined Medicaid eligibility and claims data, facility censure and program census data, consumer demographics and assessment information, consumer clinical data and more. “A lot of training has been done on taking the clinical knowledge and expertise of the care team, and combining that with the data and the information that they have available to them,” said Ms. Glavin. She went on to explain that enabling nurses to use this data has been especially beneficial.
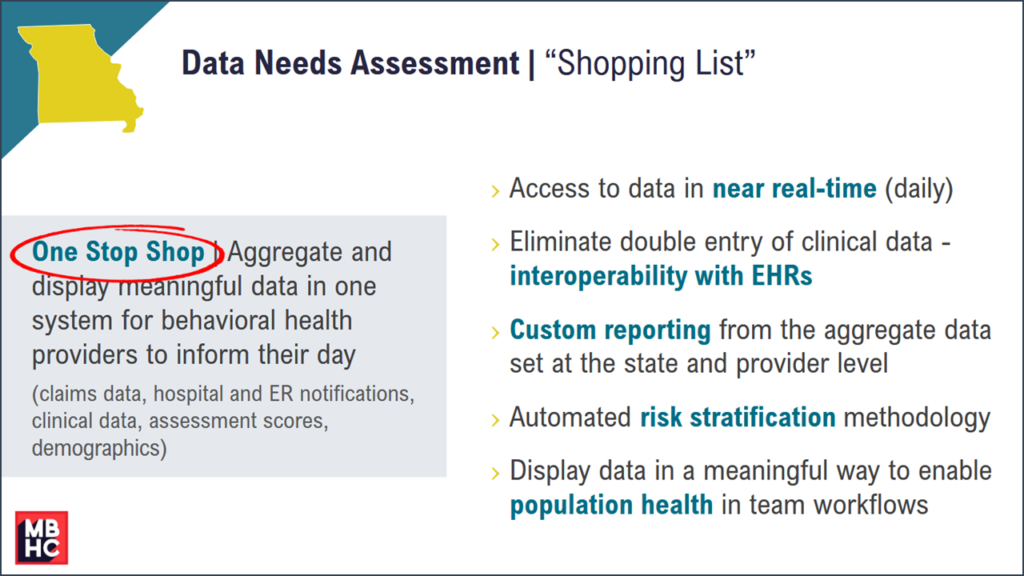
But having the data in one place is only the start. It is important to have the ability to customizing reporting at every level of the system—and get that reporting on a real time (almost daily) basis. The Missouri system is designed to both provide real time alerts to the care team of emergency room and admissions event. And the data system provides information to care managers to address consumer gaps in care. For years, “The custom reporting was another piece, it was also on the Department of Mental Health roadmap. They needed to have an ability to be able to run their own reports, providers wanted that too,” said Ms. Glavin. Until recently, they relied on excel spreadsheets, which could created a month and a half communications lag.
And beyond the consumer-centric data, to maximize system performance, managers need systems supporting managing across the population including risk stratification. MBHC set up the system to assess the population for a wide range of health risks. These risks include metabolic status and screening, medication use, use of emergency rooms and hospitals services, housing and employment status, suicide risk and other functional risk assessments.
“We’re now on the path of really pulling more data and information from the EHRs into a data warehouse. But I’m really glad that we started on the front end with care manager and designing a system that would support the work of the folks on the ground doing the work,” said Ms. Glavin, “Without that, and without giving them access to the data, solving for the things on our shopping list, they wouldn’t be able to produce all the great outcomes that we’ve been able to show in Missouri.”
