By Monica E. Oss, Chief Executive Officer, OPEN MINDS
In the 2019 report “Facing Addiction In America: The Surgeon General’s Spotlight On Opioids,” U.S. Surgeon General Jerome M. Adams, M.D., referred to medication assisted treatment (MAT) for opioid use disorder (OUD) as the ‘gold standard’. But that endorsement hasn’t been enough to drive adoption of MAT.
Despite the ‘gold standard’ endorsement, only about one in five adults with OUD received medication as part of their treatment (and only one in three received any type of treatment) in 2021. Those were the findings of a recent analysis published two days ago—Use Of Medication For Opioid Use Disorder Among Adults With Past-Year Opioid Use Disorder In The US, 2021.
The analysis also found that access to MAT was not evenly distributed. Men with OUD were six times more likely than women to receive medication. White adults were 14 times more likely to receive medication than Black adults. Unemployed adults and those living in rural areas were also less likely to receive medication for OUD treatment.
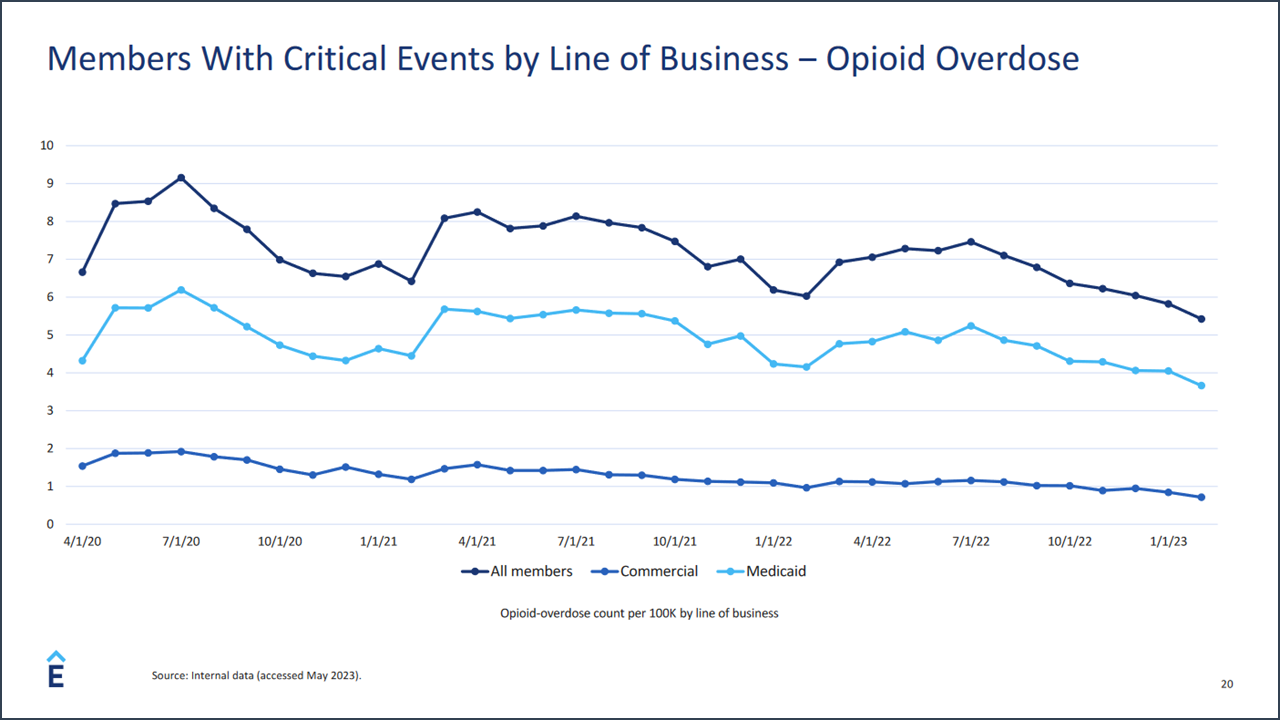
At our recent 2023 OPEN MINDS Strategy & Innovation Institute, David Lederman, Senior Product Manager for Elevance Health, spoke to another difference in MAT utilization in his keynote, Behavioral Health Advantage – The Elevance Health Approach To Innovations In Substance Use & Suicide Prevention—the differential use of MAT for substance use disorders (SUD) among the Medicaid and commercial health plan populations. Mr. Lederman attributed the 20+% difference in utilization between the two populations to a number of factors including preconceived notions about the medications and the difference in treatment provider organization philosophies.
While this research did not attribute the low use of MAT to any particular factors, there have been studies looking at the issue. There are many barriers preventing broader access to MAT for OUD including stigma, inadequate professional education regarding the use of medication, delivery system fragmentation, regulatory and legal barriers, barriers related to public and private health insurance coverage, and reimbursement and payment policies have been attributed to the situation.
Interestingly, the research found that access to telehealth was associated with an increased use of MAT. Those receiving addiction treatment via telehealth were nearly 40 times more likely to receive medications for OUD than those who did not have access to telehealth treatment.
The current low rates of utilization of MAT for OUD affecting every quarter of the health and human service field. People with untreated or unsuccessfully treated OUD fill our hospitals, our prisons, and our morgues. There are an estimated 2.5 million adults in the U.S. have an OUD. And overdoses and premature death is all too frequent in this group. Opioid-involved overdose deaths rose from 21,089 in 2010 to 47,600 in 2017 and remained steady through 2019. This was followed by a significant increase in 2020 with 68,630 reported deaths and again in 2021 with 80,411 reported overdose deaths.
Opioids also have an outsized effect on the workforce. Nearly one in five adults (18%) have received a prescription for opioids in the past year—and almost all (91%) filled the prescription and 29% refilled the prescription.
Of the U.S. workforce, receive an opioid prescription each year. A 43% decline in the men’s labor force and 25% decline for women, between 1999 and 2015, has been attributed to opioid abuse. And, workers with an SUD take almost 50% more days of unscheduled leave than other workers and have an average turnover rate 44% higher than that for the workforce as a whole.
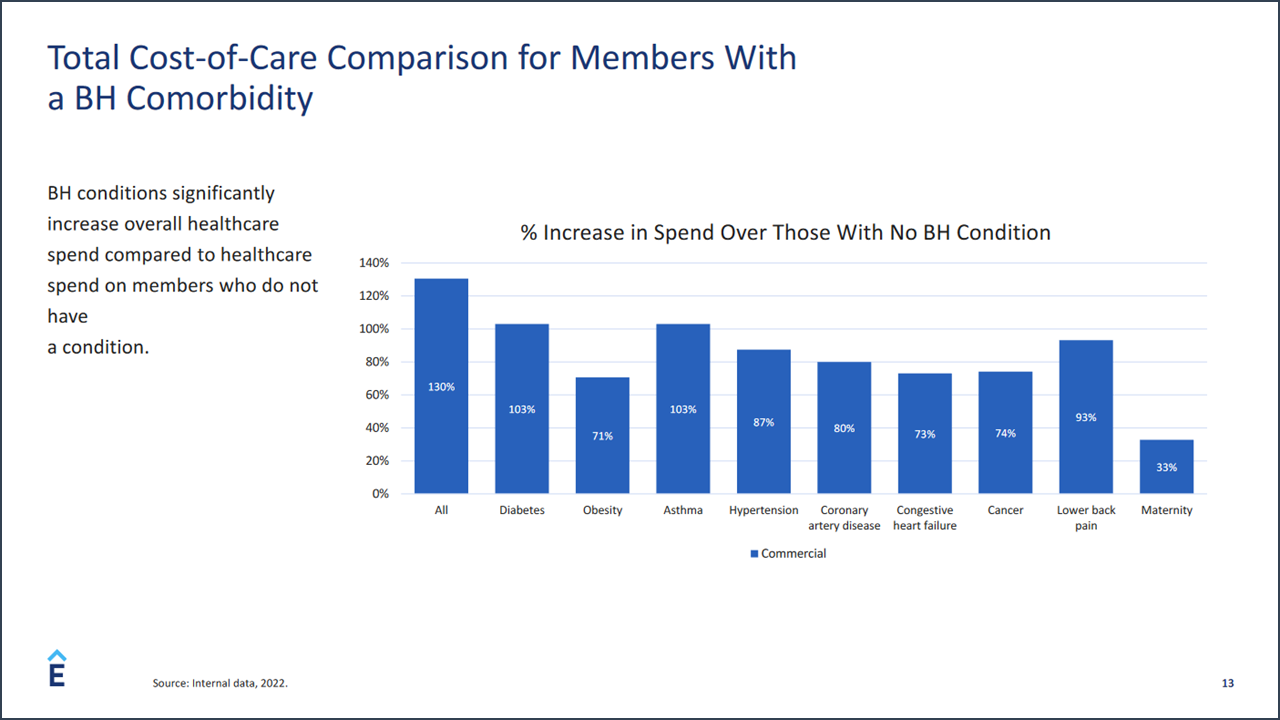
And OUD increases the use of health care resources. Mr. Lederman discussed how analysis of Elevance Health’s claims data found that the cost of medical treatment doubles for commercial health plan members with a behavioral health condition—and triples for members with an OUD. In particular, intravenous users had a 77% higher total cost of care than the average member.
This is not the first (or the last) time that we’ll see the slow adoption of innovation in treatment. Historically, there has been a much discussed (but never changed) “science to service” lag of 17 years in health care. This means that on average, it takes almost two decades for innovations in health care to become mainstream best practices.
But for the executive team of any organization that is focused on ‘whole person care’ and plans to succeed with value-based arrangements for population health management—whether a health plan, a care manager, or a provider organization—ignore the ‘gold standard’ at your own risk.
