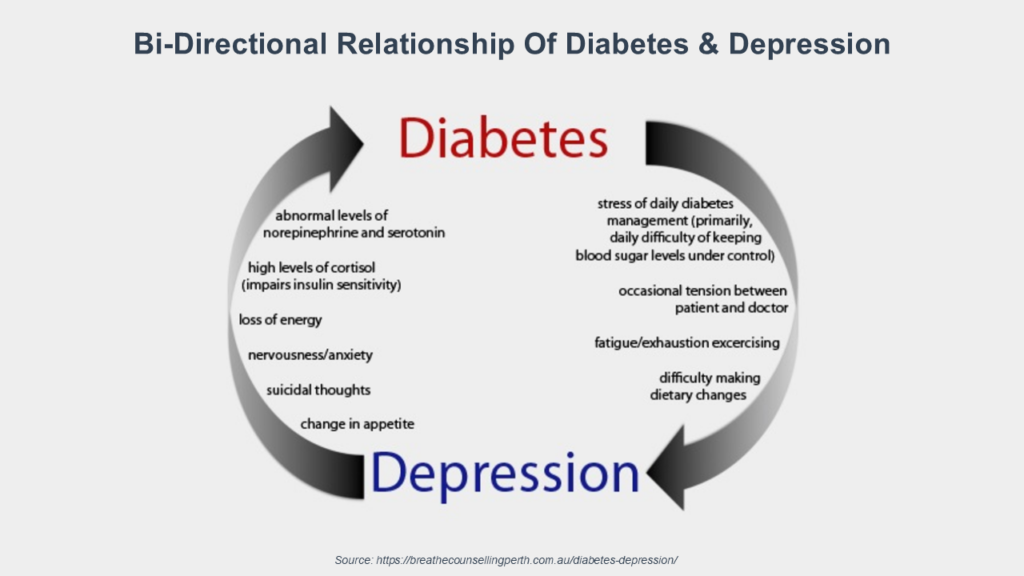
The evidence linking mental health conditions and chronic diseases continues to mount. A new study found that the prevalence of diabetes was higher in depressed than non-depressed individuals (21% versus 14%)—and that this risk increased with the consumer’s age. The study also found that a high proportion of consumers with diabetes also experienced depression.
The research supports the theory that depression affects not only the brain, but also other body systems. This includes insulin resistance, higher cholesterol levels, elevated inflammation, and bone metabolism. And there is evidence that this metabolic disturbance occurs with other cognitive disorders including schizophrenia, Alzheimer’s disease, autism spectrum disorder, and various affective disorders. For example, research has documented that serious mental illness (SMI) is associated with a two-to-threefold increased risk of type 2 diabetes.
At the same time, individuals with diabetes had a higher incidence of depression. But the research attributes this to sub-optimal diabetes management.
For consumers, this association between depression and diabetes has severe consequences. Individuals with comorbidity of depression and diabetes mellitus (DM) had a 63% lower survival rate than the average.
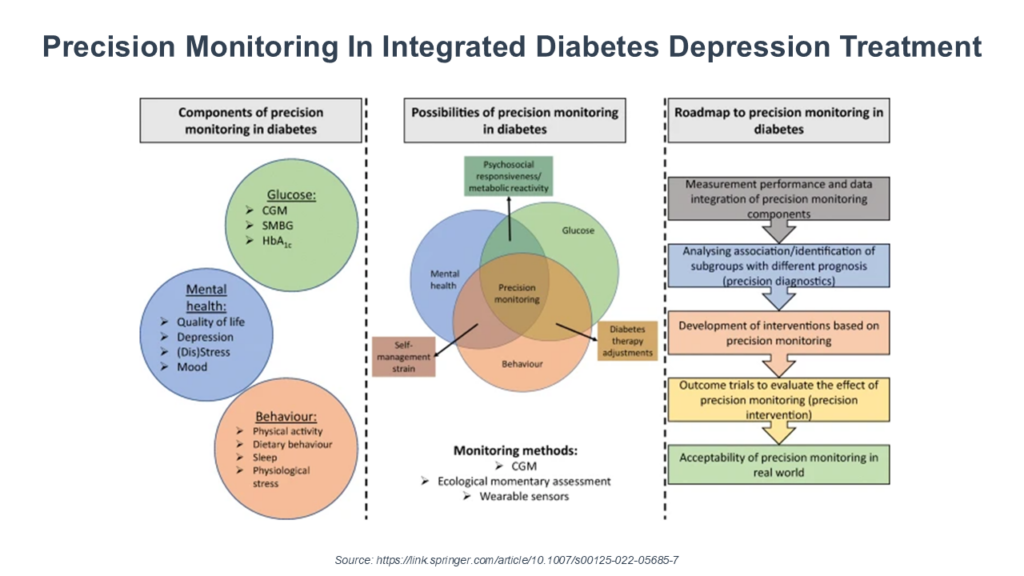
What are implications for serving consumers with mental illnesses? This research supports concept that diabetes isn’t a condition that “happens” to occur in consumers with mental illness. Rather, the mental illnesses are driving the development of diabetes. It creates an imperative to rethink the clinical model for serving consumers with mental illnesses—with a great focus on monitoring, preventing, and treating diabetes and hypertension.
This is important as the field moves to whole person care models—and to value-based reimbursement with total cost of care incentives for care coordination and community-based care. Untreated diabetes can cause heart attacks, strokes, kidney damage, amputations, and nerve damage. This translates into excess costs—$6,680 for commercially insured consumers, $4,360 for Medicaid, and $3,430 for Medicare. Diabetes, particularly untreated diabetes, drives up the total cost of care for consumers—and will reduce the margins in value-based reimbursement arrangements looking at emergency room use, hospitalizations, and/or total cost of care.
For any executive team that is currently (or planning to) move into whole person models of care, this issue calls for a rethinking of the protocols and practices managing consumer care—particularly consumers with depression, schizophrenia, autism, and dementia. There are evidence-based models to draw upon for program design—like Diabetes And Depression: Strategies To Address A Common Comorbidity Within The Primary Care Context, A Framework For Developing A Successful Diabetes Center of Excellence, Professional Education–Behavioral Health In Diabetes Care, and Patient-Centric Chronic Care Management Strategies For Diabetic Patients.
Interventions like cognitive behavioral therapy (CBT) have proven to be effective for consumers with depression and diabetes. And addressing health-related social needs (HRSN) can address the social determinants of health and access issues that contribute to poor diet and lower adherence to a diabetes-friendly diet.
This research points to the potential of ‘whole person care’ approaches to consumer health management. But for most organizations—whether on the primary care or the specialty care side of the equation—this requires a deliberate changes in design (and culture) for success.
