By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Just a few weeks ago, the U.S. Department of Health and Human Services (HHS) announced that a nationwide health data exchange was operational, providing secure transmission of consumer data across providers, hospitals, health plans, and public health agencies. Five Qualified Health Information Networks (QHINs) began exchanging data on December 12 under the Trusted Exchange Framework and Common Agreement (TEFCA)—a set of common rules for data exchange required by the 21st Century Cures Act of 2016.
This new development will move the field away from the current situation where “every pair of payers and providers has to cut through a legal and technical thicket to connect their APIs”.

The reasons for the health care policy focus on interoperability and data sharing are clear. Whole person care models improve outcomes and consumer health status—and reduce overall spending. But data sharing that consolidates all of a consumer’s health, behavioral health, and social supports information into a single record is necessary to make those models work.
In addition to the continued federal push for interoperability (something that has been less than successful for two decades), state governments are also trying to tackle this problem. We got an up-to-the-minute look at one such initiative—in California—in our recent Circle Executive Roundtable, Preparing For CalAIM: The New California Health & Human Services Data Exchange Framework, featuring Timi Leslie, President of BluePath Health, and Anwar Zoueihid, Vice President of Long-Term Care Services & Supports of Partners in Care Foundation.
BluePath Health has a contract with the California Health & Human Services Agency (CalHHS) to assist in the development of California’s Data Exchange Framework (DxF). The purpose of the DxF is to create new connections between health and social services provider organizations, requiring the secure exchange of health and human services information. California-based Partners in Care is a $28 million non-profit with a statewide network of community-based organizations providing care coordination for older adults.
California is launching their DxF with the state’s first-ever statewide Data Sharing Agreement (DSA). A wide group of organizations—including general and psychiatric hospitals; physician practices and medical groups (with >25 physicians); skilled nursing facilities and clinical laboratories; and health care service plans and disability insurers—are required to sign the DSA by January 31, 2023, and are required to begin exchanging information or provide access by January 31, 2024.
Ms. Leslie spoke to the importance of the data exchange in supporting some key initiatives of CalAIM—Enhanced Care Management (ECM), community supports, and population health management. Each of these requires a whole person approach to care, and the ability to share consumer-specific information. Unique to California is the inclusion of community-based organizations (CBOs) and their social support services in a Medicaid consumer roadmap.
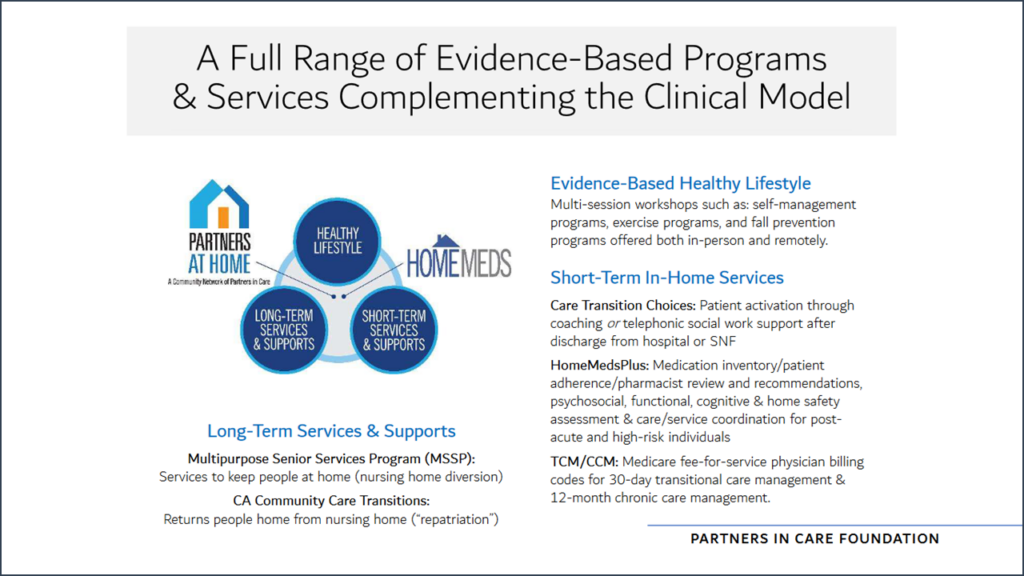
Mr. Zoueihid presented a case study of how this works in practice. He described the CBOs in the Partners in Care network as serving as a bridge between medical care and what a person accomplishes in their own home. “We manage the gaps in non-medical care that affect a person’s recovery and overall health,” Mr. Zouehidi explained. The CBOs provide in-home service coordination, caregiver support, and consumer education. This approach includes programs encouraging exercise and self-management of chronic conditions. And the CBOs provide medication management services via “plug-and-play” software that documents inventory, adherence issues, and insight to pharmacists. And the organization manages care transitions when Medi-Cal members return home after hospitalizations.
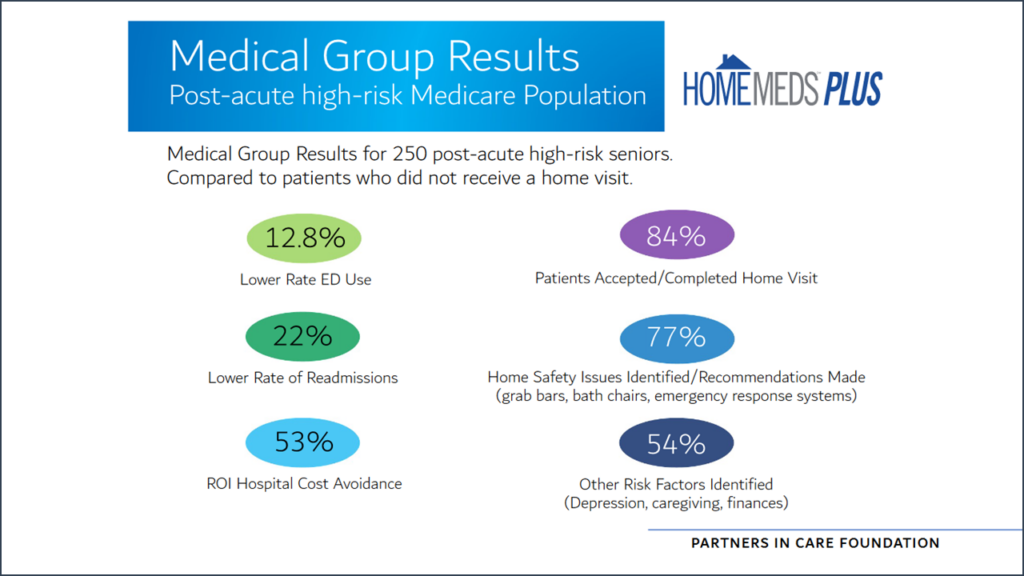
The initial performance data for the CBO interventions are impressive. This includes a 13% lower use of emergency room services and a 22% lower hospital readmission rate.
Mr. Zoueihid stressed the importance of data sharing in their success: “Our vision is to expand care coordination through data exchange and streamlining the care coordination process.” The DxF exchange allows the automation of care coordination with real time access to consumer data. “This gives us a more proactive care approach in terms of data outcomes and metrics,” said Mr. Zoueihid. “We see the lower readmission rates promoting population health equity. This is a really big case of the data exchange framework supporting seamless care coordination with person-centered data to ultimately improve health equity…The way we are working now, in non-siloed ways, to exchange this data is really providing a lot of good outcomes so far.”
As the improved performance resulting from data sharing become better known, there will be more pressure on all provider organizations, care management entities, and health plans to participate. Ms. Little discussed how the state of California is providing funding to make data sharing a reality. California has set up DxF grants to help all provider organizations determine how to engage in the data sharing agreement and what the requirements are. A technical assistance (TA) grant is available to pay for internal or external consulting to help provider organizations determine how they can best integrate with the DxF. The grants can be used for consultation or to cover the cost of onboarding with a QHIO to share data.
CalAIM CITED and the Incentive Payment Program (IPP) are two funding opportunities that are opening in the first quarter of 2024. CITED funding is for provider organizations providing ECM and community support services to expand their capacity and infrastructure to integrate with the DxF. IPP funding is available to provider organizations through managed care plans. These TA funds are available through 2027. “The state has set up funding mechanisms to help organizations that are new to this data sharing world build the necessary capacity, both in terms of people, process, and technology,” said Ms. Little.
For over two decades, discussions of interoperability have always been predicated by a discussion of why it can’t happen. These state and federal initiatives are going to make data sharing a reality—and the competitive organizations will be the ones that leverage that new data for better value in consumer care. “The new data exchange framework is the first step towards creating a road map for full statewide data exchange processes in the coming years,” observed my colleague Richard Louis, OPEN MINDS Vice President. “Provider organization executives will need to plan now to have the right technology for the future.”
