By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Executives of health plans agree that 35% of total health care resources are used by the 5% of the population with a behavioral health disorder. What they don’t agree on is the best way to manage the care of those consumers—that’s where population health gets complicated.
The data is very clear—for consumers with mental health conditions, substance use disorders, intellectual and developmental disabilities (I/DD), autism, and more. A new study—Real-World Health Care Costs And Resource Utilization Associated With Mild Cognitive Impairment In The United States: A Retrospective Cohort Study Of Commercial And Medicare Data—just adds to the evidence base.
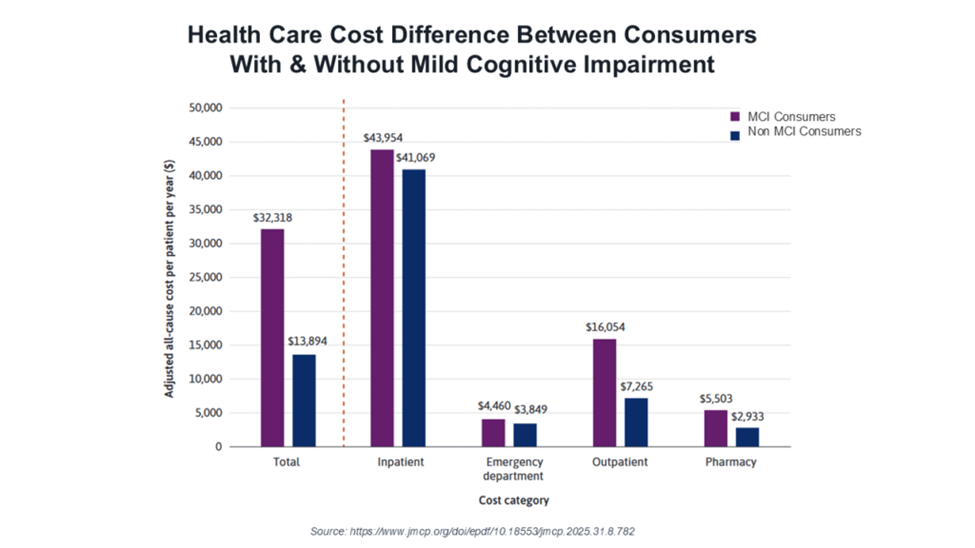
This new analysis found that individuals with a mild cognitive impairment (MCI) had total annual health care costs that were more than double those of individuals without MCI, at $32,318 versus $13,894. (MCI is a condition occurring before an individual develops Alzheimer’s disease (AD) or other dementias, causing some memory loss but not affecting daily activities.) The consumers with an MCI had higher average annual spending in every category—$43,954 versus $41,069 for inpatient, $16,054 versus $7,265 for outpatient, $4,460 versus $3,849 for emergency department (ED) use, and $5,503 versus $2,933 for pharmacy.
The authors note that the link between AD and increased total cost of care is well established and those costs increase disease severity. However, the economic burden of MCI is less understood. They believe that a potentially effective method for identifying individuals within a large population who are at risk of developing MCI, AD dementia, and other dementias is to use electronic health records (EHRs) and/or claims databases. However, these models are not yet developed.
This analysis is one of many that point to the complexities of population health management for consumers with complex conditions and social support needs. And as provider organizations and health plans develop more reimbursement arrangements that share financial risk, the ability to understand these relationships will be increasingly important in rate setting, in managing medical loss ratios, and in maximizing reimbursement under value-based reimbursement arrangements.
