In March of this year, the Centers for Medicare & Medicaid Services (CMS) announced the creation of a new Accountable Care Organization (ACO) model—focused on team-based, person-centered primary care. The model, called ACO Primary Care Flex, is a voluntary model that will focus on primary care delivery in the Medicare Shared Savings Program. The new model will test how prospective payments and increased funding for primary care in ACOs affects performance. The new model will start on January 1 of 2025.
“By giving ACOs more flexibility and additional funding and support to deliver high-value primary care, the ACO PC Flex Model can help providers identify and address people’s unmet health-related needs,” said Liz Fowler, CMS Deputy Administrator and Director of the CMS Innovation Center, in a statement. “This model strengthens incentives for more providers to form ACOs and meet CMS’ goal of increasing the number of people with Medicare who are in an accountable care relationship.”
In May, CMS issued an RFP for grant funding to support development of the new model—Federal Government Announces ACO Primary Care Flex Model Grant Funding. The grant will include a one-time Advance Shared Savings Payment to help cover costs associated with forming an ACO (where needed) and administrative costs of model implementation. It includes monthly prospective payment arrangements to move participants away from fee-for-service/visit based arrangements toward population-based payment mechanisms. The grant applications closed in August—applicants will be notified of their acceptance to participate on October 1.
This ACO PC Flex Model is just the most recent iteration of ACO models. Medicare ACOs were created as part of the Affordable Care Act in 2011. Originally, the Medicare ACOs were created to provide a structure for provider (clinicians, hospitals, etc.) collaboration on coordinated high-quality care—avoiding unnecessary services and medical errors.
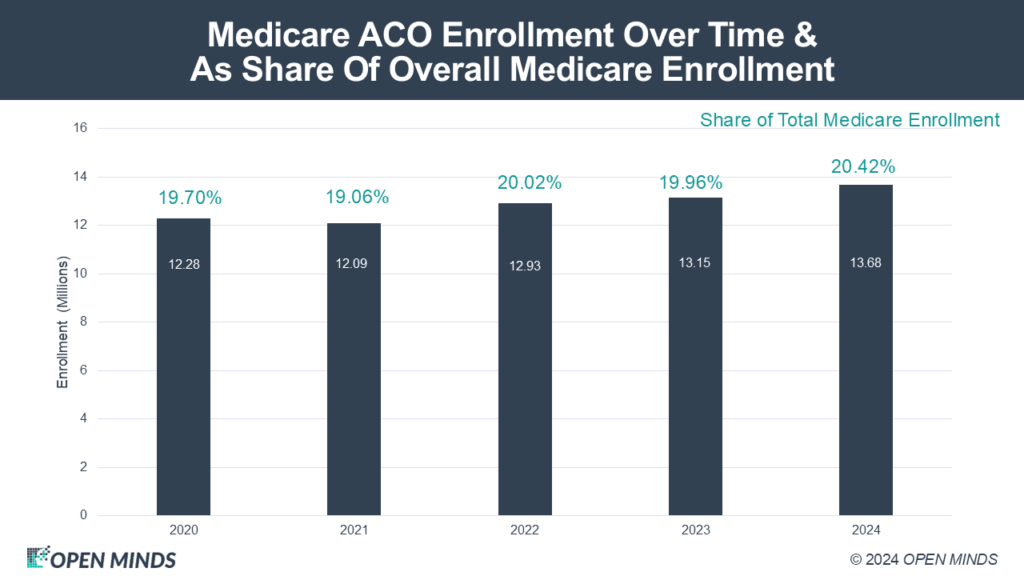
There are now 702 Medicare ACOs in operation with 13.6 million members, 20% of Medicare beneficiaries. There are currently three types of Medicare ACOs in operation—the Shared Savings Program, the REACH Model, and the Kidney Care ACO. The Medicare Shared Savings Program ACO (MSSP) model has 10.80 million enrollees as of January 2024. The ACO REACH model—with incentives for addressing underserved communities and addressing health disparities—has 2.6 million enrollees. The Comprehensive Kidney Care Contracting ACO—focused on late-stage chronic kidney disease and end-stage renal disease—has 282,000 enrollees.
The Shared Saving model saw enrollment slightly increase in 2022 by 3% to 10,418,297, compared to the 2021 number of assigned beneficiaries of 10,124,325. A review of these ACOs shows the majority (59% of ACOs covering 64% of beneficiaries) were in a two-sided risk arrangement, while 41% were upside-only. The program saw more than $1.8 billion in net savings, and the number of federally qualified health centers participating increased by 18%.
As of June 2024, the ACO REACH program provides care to over 2.6 million traditional Medicare beneficiaries—a 24% increase in covered lives compared to 2023—with 122 participating ACOs. The ACO REACH model is scheduled to sunset at the end of 2026. CMS is currently exploring ways to integrate the successful elements of ACO REACH into other models.
The ACO developments in Medicare are critical to the planning for every health and human service executive team. Medicare members are now 18.7% of the adult U.S. population—and Medicare spending is 21% of the total U.S. health care spend.
