By OPEN MINDS Circle
New models of care coordination for consumers with complex needs continue to move ahead—the Center for Medicare & Medicaid Services (CMS) just announced that four states will be participating in the Innovation in Behavioral Health (IBH) Model. The eight-year IBH program will be launched through state Medicaid agencies in Michigan, New York, Oklahoma and South Carolina (see ‘CMS Launches New Program For Mental Health, OUD Treatment’). Oklahoma will implement the model statewide, while Michigan, New York, and South Carolina will implement it in designated sub-state geographic service areas.
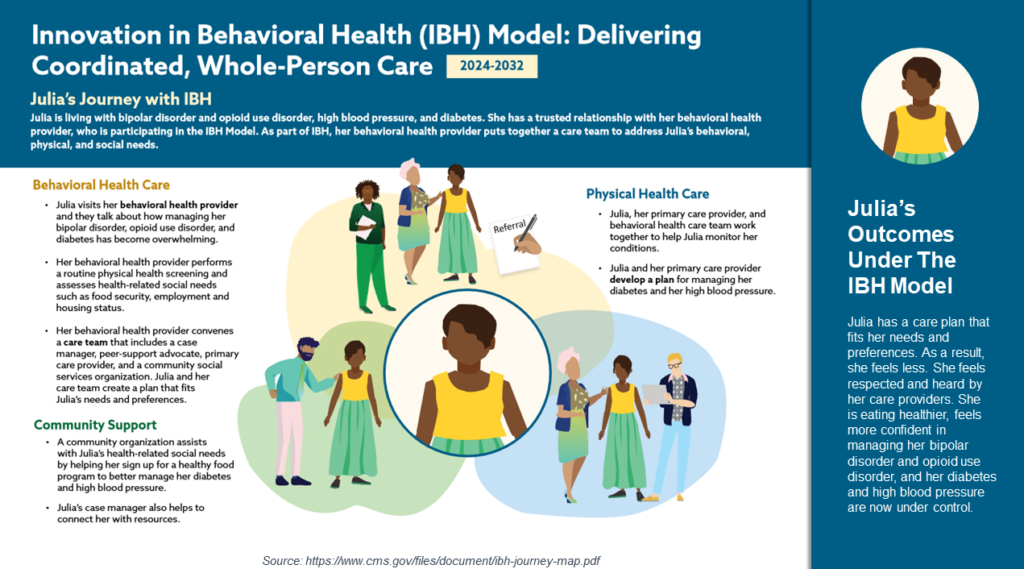
The IBH model is focused on care management for consumers in Medicare and Medicaid plans (dual eligible or not) dealing with severe mental health conditions and substance abuse disorder (SUD) or both. Provider organizations able to participate include community mental health centers, opioid treatment programs, and public or private practices. The requirement is that the participating provider organizations manage the behavioral, physical health, and health-related social needs of participants (see ‘One More Integrated Care Model’ and ‘CMS Starts Accepting State Applications For Medicaid ‘Innovation In Behavioral Health’ Model’). Reimbursement will include a value-based care approach, with compensation based on quality of care provided and improved patient outcomes.
The IBH model moves the health care field closer to true integration of primary care and behavioral health. It is similar to the total cost of care model being implemented by Centene’s Sunshine Health Plan in Florida.
These models are both an opportunity and a threat for traditional provider organizations, as the effects on market share in any particular market are significant. On the opportunity side of the equation, the model opens up new revenue for the selected provider organizations for the services for assigned consumers—and the ability to participate in value-based contracts that offer more flexibility in service delivery (including the use of collateral technologies) and share of savings in total cost of care.
But these models also challenge market share. With a model that assigns consumers to a particular provider organization for their primary care and behavioral health services, the total available market for those services shrinks with every contract. For the assigned consumer, those primary care services and behavioral health services will either be delivered by that provider organization or by a provider organization in their subcontracted network. The primary care and behavioral health services consumers are no longer “available” to the market.
Look forward to more information on care coordination and integrated care from ONEcare Population Health Academy, sponsored by Alera Health, in partnership with OPEN MINDS.
