Last month, the National Committee for Quality Assurance (NCQA) announced changes to how follow-up after mental health-related emergency department visits and hospitalizations is measured in its Healthcare Effectiveness and Data Information Set, known as HEDIS. The measure is one of the most important indications of the state of continuity of care in a health care delivery system. The changes—in both the team members who can facilitate continuity of care and the settings—reflect the growing dominance of integrated care models and hybrid care delivery for consumers with behavioral health conditions.
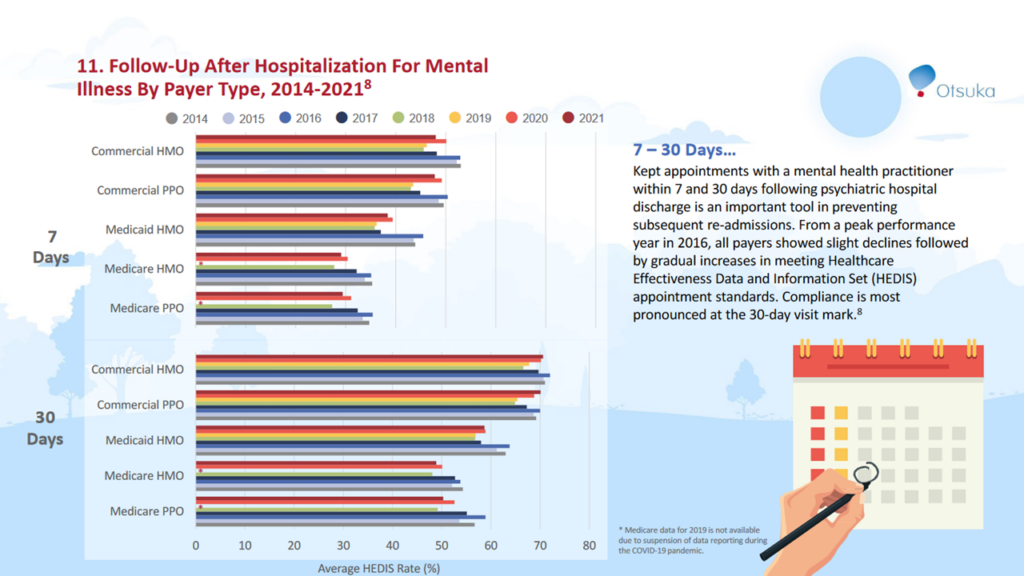
The HEDIS follow-up measures are at both 7 days and 30 days after a consumer is discharged—and is measured across commercial plans (HMOs and PPOs), Medicaid HMOs, and Medicare plans (HMOs and PPOs). Over the past ten years, health plan performance on these two measures has varied. Not surprisingly, commercial health plans have better rates than their Medicaid and Medicare counterparts.
A recent study found that hospitalization follow-up among youth and young adults with private insurance was 42.7% within 7 days and 64.7% within 30 days. Of those with emergency room use, 28.6% received follow-up within 7 days and 46.4% within 30 days.
The new rules expand the conditions where follow-up is required for phobia diagnoses, anxiety diagnoses, intentional self-harm X-chapter codes, and the R45.851 suicidal ideation code. This is in addition to the current list of conditions—schizophrenia spectrum and other psychotic disorders; bipolar and related disorders; depressive disorders; obsessive-compulsive and related disorders; dissociative disorders; personality disorders; disruptive, impulse control and conduct disorders; as well as trauma-and-stressor-related disorders.
The rules also changed who can provide follow-up care. Previously, only a specialty mental health professional could provide that follow up. Going forward, follow up can be provided by peer support specialists and primary care professionals. And that follow-up can now occur in psychiatric residential treatment setting in addition to the outpatient visits, and intensive outpatient or partial hospitalization. Importantly, the follow-up can also happen by telehealth and telephone visits.
My colleague, OPEN MINDS senior associate, Sharon Hicks observed, “I think that NCQA has really moved in the right direction with this change. Treatment for serious mental illness and for significant substance use disorder has always comprised many services provided by professionals other than licensed behavioral health clinicians. The role of these team members has been to support medical treatment, but also to provide education, recovery support, and services associated with health-related social needs. NCQA’s modification to the measurement for this standard will allow organizations to do a more effective job of coordinating care post discharge which will, hopefully, result in better continuity of care.”
Why does this matter? HEDIS scores affect health plan contracts, bonuses, and enrollment—and have the attention of executives in health plans and across the field. The challenge is that most provider organization executive teams don’t know how their organization stacks up on these measures for the consumers they serve. In many cases, health data system interoperability plays a role in this disconnect—with community-based provider organization managers not having data on consumer hospitalizations or medications. But it is critical for executive teams to find a workaround for having access to consumer information relevant to the HEDIS measures.
Margaret Mays, my colleague here at OPEN MINDS, sees challenges and opportunities in the new measures. “The new changes have both positive and negative effects on health plans. While changing to any clinical professional will count as a follow-up visit and can result in an increase in rates, NCQA has also expanded the denominator to include previously excluded conditions. Intervention strategies will need to be re-evaluated and reworked to accommodate the changes. At the same time, these changes will hopefully allow provider organizations more flexibility in scheduling follow-up visits—in types of team members and types of setting. To address this measure’s expanded population, provider organizations need to ensure they have programs or interventions in place for monitoring and ensuring follow-up after an emergency room visit.”
The challenge coming is that the new rules should significantly improve the usefulness of the HEDIS scores for follow-up after hospitalization—and the baseline required for competing on performance. That is a win for consumers.
