By Monica E. Oss, Chief Executive Officer, OPEN MINDS
The past year has seen some notable changes in the U.S. health care delivery system—changes that directly affect the future revenue of specialty and primary care provider organizations. Topping my list of the developments with strategic impact are the expansion of retail clinics into behavioral health, the expansion of home care companies into specialty services, the growth of virtual and in-home health care provider organizations, and the ‘backward’ integration of health plans into service delivery.
For traditional provider organizations, these developments are likely to result in a shift for consumers with less complex mild and moderate conditions to these new care delivery options. The key to maintaining revenues and continued growth is a focus on consumers with more complex conditions and complicated support needs—the 20% of consumers that use about 80% of resources each year. These consumers have not been well-served in most markets—and the opportunities for innovation using whole person care approaches and new technology in value-based program models is substantial.
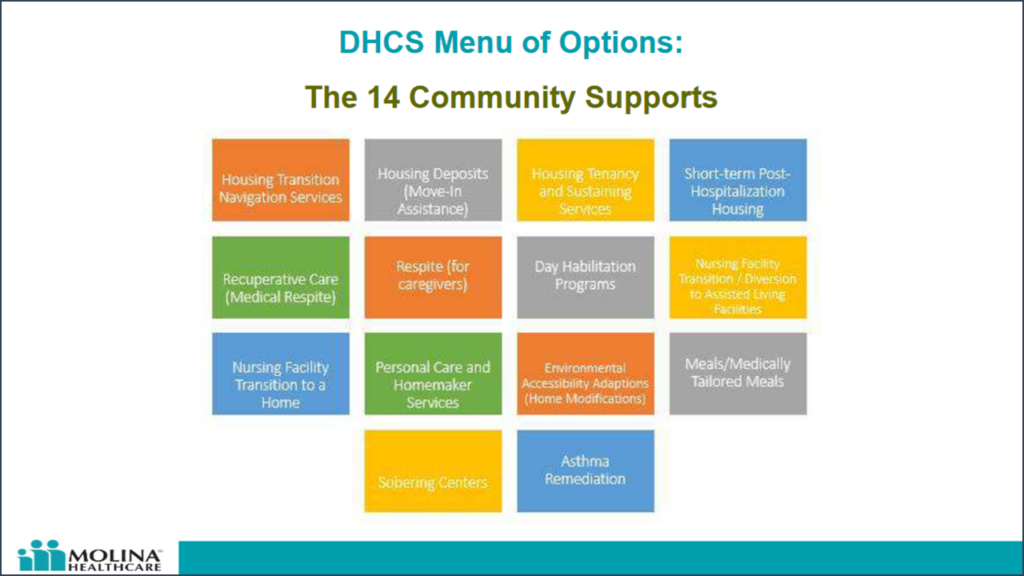
Our recent OPEN MINDS Circle Executive Roundtable, Preparing For CalAIM – Expanding Health Plan Contracts With Managed Care Plans For Complex Medi-Cal Youth, focused on these emerging market opportunities. Neeta Alengadan, Associate Vice President of Healthcare Services, Molina Healthcare of California, and Eric Schwimmer, Director for Enhanced Care Management, Anthem Blue Cross, spoke of the new opportunities to provide community supports and enhanced care management (ECM), also known as in lieu of services (ILOS), for high-need consumer groups. To make this happen, they touched on three critical elements that provider organization executives need to be prepared to address and demonstrate to bring new solutions to health plans—participation in a collaborative contracting process, clinical data exchange functionality, and population health management capabilities.
Participation In A Collaborative Contracting Process—Not all provider organizations are as prepared to deliver services as health plan managers think they should be. Entering into the contracting process—particularly with new services—executives should be prepared to demonstrate their capabilities and discuss the current and projected performance of new services they are proposing. Some of the other required information includes program descriptions, technology functionality, referral arrangements, data sharing capabilities, and clinical staff National Provider Identifiers (NPI) and licensure information.
“We’re not looking to exclude provider organizations,” said Mr. Schwimmer, discussing their provider contracting process for Medi-Cal. “We’re looking to build you up, make it work, and have you join our network. When you submit a complete application, what we call a certification application, our clinical team reviews the application. They work with you to address the gaps until they’re confident that you can do the job. It’s a very collaborative process. Once you pass that phase, you go to our credentialing and contracting teams to complete the administrative part of the application process. End to end, the whole process can take about six months.”
He continued, “When you get to the certification process, that is generally the hardest part… There has to be evidence for our clinical team to see that shows you have a deep and substantial experience serving the population of focus that you are intending to serve. They want to see that you have the capacity to keep good records. They want to see things like Memorandums of Understanding with other provider organizations that might help you serve consumers better.”
For more on preparing for the health plan contracting process, check out The OPEN MINDS Managed Care Competencies Assessment and How To Build (& Succeed With) Value-Based Payer Partnerships: An OPEN MINDS Executive Seminar On Best Practices In Marketing, Negotiating & Contracting With Health Plans.
Clinical Data Exchange Functionality—Whole person care approaches to care coordination have historically been stymied by the lack of electronic health information exchange (HIE). Lack of consumer data across the delivery system is an impediment not only to care coordination but also to success with value-based reimbursement (VBR) arrangements. In our recent survey, the most common performance measures included readmission rates, emergency room presentations, and follow-up after hospitalization—all requiring a broader consumer information set.
But there are many options open to provider organization executive teams to build the clinical data needed to coordinate consumer care—ranging from participating in state or local HIE initiatives to bi-directional data exchange with specific provider organizations.
Discussing the provider interoperability requirements in California’s Medi-Cal program, Mr. Schwimmer said, “DHCS has an ambitious program to help all Medicaid provider organizations adopt data exchange standards and enable bidirectional data sharing with the health plans and health information exchanges… They are calling it social health information exchanges. This is super exciting work. We’re looking for the provider organizations that either have that capacity already or are willing to work with us to build that capacity.”
Population Health Management Capabilities—Finally, the ability to manage the health of a group of consumers across medical, behavioral, and social domains is a key to success in this new environment. Most programs for these more complex consumer groups are only going to be financially sustainable with a funding mechanism other than fee-for-service—and that requires new infrastructure capabilities.
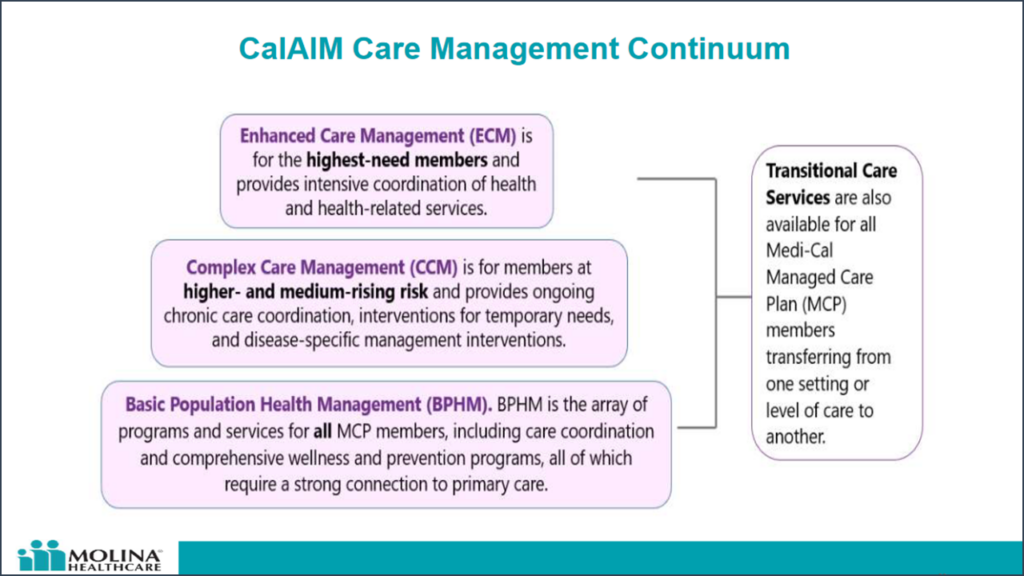
“With the new population health management strategy, you have what was called basic care management that dovetails into basic population health management and tiering members in terms of what risk level they’re at,” said Ms. Alengadan. “A big part of that is transitional care, outreach, and engagement. We’re looking at that across the board for all care settings. There needs to be strategies and an ECM lead care manager that can coordinate all of that.”
The shift in the market is creating challenges in competing for consumers and health plan contracts for many provider organization executive teams. But the emerging market for supporting the high-needs consumers is a growth opportunity in the decade ahead.
