By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Specialty provider organizations start the new year with a few tasks on the to-do list: tackling margin compression, increased competition, and the evolving expectations of payers and consumers, all while crafting a financially sustainable vision for the future. That includes developing next-generation services that address the demands for hybrid and whole-person, growing cash reserves to support value- and risk-based reimbursement models with payers, and maintaining (or growing) the right leadership and management team while keeping staff positions filled.
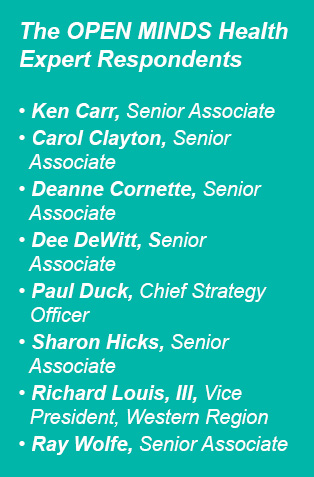
So, how do the executive teams of provider organizations serving complex consumers address the financial challenges and identify growth opportunities in this new year? I decided to find the answers by asking my expert colleagues at OPEN MINDS. I posed two questions to them:
- What are the biggest financial sustainability challenges specialty provider organizations will face in the next two years?
- What are the revenue growth opportunities for providers in the same period?

Financial Sustainability Challenges
As I spoke with each of my colleagues, three key financial sustainability challenges developed:
- Shrinking profits and cash reserves: This appears to be the number one challenge for specialty provider organizations in maintaining overall profitability and increasing cash reserves. With razor-thin margins, little cash, and limited credit, many providers risk failing without a major shift in strategy, an influx of investment, or some form of partnership.
- Difficulty in hiring and retaining qualified staff: The second challenge is pervasive in health care and other industries—just filling open positions (let alone with highly qualified candidates). Many providers report revenue constraints due to continuous staff vacancies, limiting their service capacity to meet market demand.
- Lack of funds for investment in new services and innovation: The third financial challenge is often overlooked; with limited margins, reserves, or access to credit, specialty providers cannot budget for the innovation and new service research and development critical for pivoting to meet shifting market demands.

Here’s a look at what each of my colleagues had to say.
Carol Clayton, OPEN MINDS Senior Associate. The biggest challenge for provider organizations is shrinking profits, making new service exploration and the ability to try new things (and fail) difficult. Without the revenue to invest in business opportunities and innovation, provider organizations will grow smaller and have a “just staying alive” business model, getting smaller and smaller year over year.

Dee DeWitt, OPEN MINDS Senior Associate. One of the biggest challenges for non-profit provider organizations is their average number of days with cash on hand. Historically, it has been difficult for organizations to build needed cash reserves. With the need to invest in new technologies to stay contract-compliant, reserves to accept at-risk contracts, and escalating costs (particularly labor), a key challenge will be sustaining service levels while investing for the future.

Sharon Hicks, OPEN MINDS Senior Associate. Expenses associated with human capital have always been the highest line item for almost any clinical service delivery program, and this expense will likely rise over the next two years. The competition for master’s-level, licensed staff will grow, and salaries, bonuses, and incentive payments will add expenses. In addition, the salary expectation for psychiatrists and addictionologists is climbing based on the scarcity of these professionals.

Richard Louis, OPEN MINDS Executive Vice President, Western Region. One of the biggest challenges is the payer (public sector and health plan) shift towards whole-person care models of service delivery under increasing performance and value-based approaches. Provider organizations must invest some capital and reallocate resources over the coming years to build new service delivery models to meet these new payer expectations. Those who can achieve this will thrive in their markets (both in market share and preferred payer relationships); while those who cannot are risking increased financial instability and will find financial sustainability through strategic partnerships. In the end, there will be some that go out of business.

Ray Wolfe, OPEN MINDS Senior Associate. An ‘organization strangulation’ is occurring in the income statement caused by a constriction in revenue, increased staffing costs, and other expenses. The badly needed new projects for long-term sustainability are being curtailed to assure short-term survivability. There is no room for error and, in many cases, no room for initiative.
Revenue Growth Opportunities
So what are specialty provider organizations to do with so many challenges affecting financial sustainability? I again turned to my colleagues for ideas on emerging revenue growth opportunities for specialty provider organizations.


Ken Carr, OPEN MINDS Senior Associate. The ability to implement new emerging service lines doesn’t happen without a dedication to innovation planning, leadership guidance and support, and resources. The checklist for evaluating new services should focus on those that demonstrate value, are technology-enabled, and integrate with a whole-person care focus.
Deanne Cornette, OPEN MINDS Senior Associate. To maximize growth potential, specialty providers should be looking to:
- Expand telehealth services: Telehealth services are rising, especially in behavioral health. Expanding or enhancing telepsychiatry and teletherapy can allow behavioral health providers to reach underserved areas and improve patient accessibility.
- Implement models of integrated / whole person care: Integrating mental health services with primary care can maximize patient outcomes and provide a more comprehensive approach to health care. In addition to partnering with primary care practices, behavioral health providers can consider co-locating their services.
- Population health management: By identifying and addressing the mental health needs of specific populations, behavioral health providers can engage in population health management strategies. Health care costs can be reduced and outcomes improved by targeting early intervention and preventive interventions.
- Specialized programs for specific demographics: Creating specialized programs tailored to specific demographics, such as children, adolescents, or the elderly, can meet the unique needs of these populations. This may involve developing targeted marketing strategies and collaborating with community organizations as well as payers.
- Increased services for substance use treatment: Substance use issues are becoming more widespread, and effective treatment programs are in increasing demand. Behavioral health professionals can enhance or expand treatment and recovery from substance use.
Dee DeWitt, OPEN MINDS Senior Associate. Providers that are excellent at managing complex, chronic behavioral health populations are in an excellent position to expand commercial revenues as more health plans become responsible for SMI and SED populations. Similarly, organizations that can provide combined behavioral health care and primary health care are well-positioned for growth, particularly in value-based payment arrangements.

Paul Duck, OPEN MINDS Chief Strategy Officer. I see two growth opportunities with payers specifically. The first is partnering with managed care organizations (MCOs) and offering services to reduce inpatient hospital expenses by aiding in hospital diversion, discharge transition, and follow-up after psychiatric hospitalization. Secondly, specialty providers can partner with payers to broaden access to care, especially for the severely mentally ill population, where making community-based crisis care available is critical.
Sharon Hicks, OPEN MINDS Senior Associate. I see two areas with growth opportunities: 1) specializing in providing comprehensive services to persons with significantly complex needs; and 2) serving the aging population. We know that a small group of consumers with high service needs represent a large percentage of the overall spend, so specialty provider organizations that can focus on that population and are able to wrap needed services around that group of consumers can command higher reimbursement and shared savings opportunities. This small but fragile consumer population requires significant care planning and coordination. With the over-65 population growing, we can also assume that providers specializing in this population will see increased service demand. One of the areas in which this population has been underserved is substance use intervention.
Richard Louis, OPEN MINDS Executive Vice President, Western Region. Many specialty providers have successfully explored niche markets as a source of new and/or stable revenue growth opportunities. Leveraging specific service or program strengths (innovations) and growing that service line in high-demand markets allows one to stand out as a specialist. This is becoming increasingly appealing to payers looking to shore up network services for their members and specialty providers trying to find a new market position in their local market.
As payer reimbursement is increasingly coming from managed care plans (i.e., Medicaid MCOs, Medicare Advantage (MA)) and plans are expanding coverage to new treatment populations as part of new member growth strategies (I/DD, justice-involved, homeless, pregnant women, foster youth transitioning from foster care, older adults), there are new sources of revenue for providers interested in delivering services to new treatment populations. For example, an adult community mental health treatment provider can move into serving a justice-involved population or obtain Medicare certification to obtain MA contracts to serve the growing older adult market.
Ray Wolfe, OPEN MINDS Senior Associate. The greatest growth opportunities lie in mergers and collaborations with high-end medical and social service providers. Mergers within the industry (a specialty provider with another specialty provider) are not adding strength or diversity to the revenue lines for the combined organization.
Taking a look at all my colleagues have shared, I see four key areas for growth emerging:
- Expanding technology-enabled services
- Implementing models of integrated, whole-person care
- Specializing in select consumer populations with complex and chronic conditions
- Partnering with health plans and large health systems
So, my advice? Digital transformation is a mandate for specialty providers. Only technology will permit the cost-effective transformation of the experience of and relationship with the consumer. But it’s not about the technology itself; it’s about competing for consumers and managing performance metrics.
Integrating primary care into your service model and treating the “whole person” is essential and will likely aid in the behavioral health outcomes that are core to your mission. In addition, this strengthens your connection to the specialty provider niche by being able to deliver high-quality care to consumers with life-long, chronic (and expensive) conditions. It also becomes vital when you contract with payers to provide whole-person care to a specialty population with chronic conditions.
My final piece of advice echoes and summarizes the others: specialty providers need to have relationships with and partner with key stakeholders—health systems, payers, and MCOs—that support your organization’s operation as the sole niche provider for a select specialty population.
