By Joe Naughton-Travers, Senior Associate & Executive Editor, OPEN MINDS
The reach of health plans is increasing, and specialty provider organizations are paying attention. More complex populations are moving to managed care through health plans. Health plans are now covering more services. Over 75% of Americans with any type of insurance have their health benefits managed by some type of health plan, accountable care organization, or specialty benefit management company. That includes 85% of Medicaid enrollees, 95% of people with employer-sponsored plans, and 40% of Medicare beneficiaries.
Additionally, health plans’ expectations of their relationships with provider organizations have changed. For health plans, the “ideal” service delivery model has medical, behavioral, and social needs addressed together in a system that has seamless consumer services, integrated data at the consumer level, and alignment of financial incentives—think value-based and risk-based contract models.
From the provider organization’s executive team’s perspective, the question is to determine—even if your organization can’t be the entire solution—how to create (through new capability development, mergers, or collaboration) a service system with these characteristics. It is essential that you establish and cultivate your relationships with health plans and that you have the internal processes and staff to make this happen.
To address this issue, the team at OPEN MINDS has developed a three-phase framework for sustainable health plan relationships:
- Phase One: Establish the right set of health plan contracts—the right plans, the right services, the right rates
- Phase Two: Optimize health plan contracts and health plan contract management
- Phase Three: Evolve health plan relationships into financially aligned partnerships
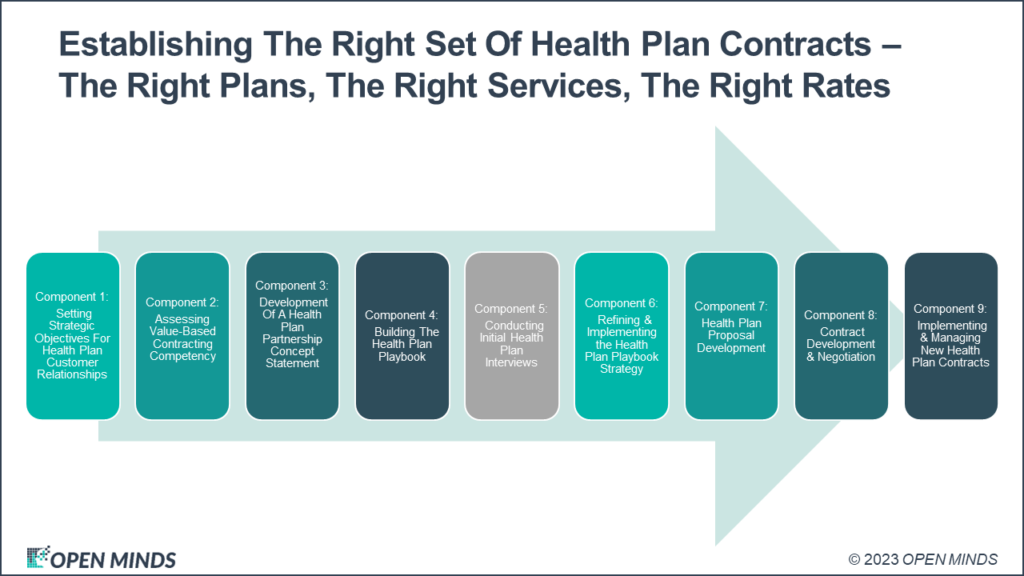
This framework is an iterative process to assure optimum revenue and solid margins in a changing health and human service landscape. This article is focused on the first phase—the process for developing the right set of health plan contracts. That framework is a nine-step process for developing relationships with health plans, from setting the strategic objectives for these relationships all the way through implementing and managing new health plan contracts.
Setting Strategic Objectives For Health Plan Customer Relationships
The first component of Phase One is to develop your strategic objectives for your relationship with health plans. Your organization’s vision and strategy for new growth and entry into new markets are what drive this phase. The focus when thinking about health plans should be on program innovations, integrated or coordinated care approaches, and achieved outcomes (e.g., are you looking to be a preferred provider with a particular health plan or to offer an innovative program model?). Along with the strategic objectives, there should be marketing objectives for the health plans.
Assessing Value-Based Contracting Competency
The second component of Phase One is formally assessing your organization’s capabilities to deliver services the way that health plans want them—under managed care and value-based contracting models. According to the Welcome & Announcement Of The Results From The 2022 OPEN MINDS Performance Management Executive Survey, 40% of specialty provider organizations reported participating in a value-based reimbursement (VBR) contract (an increase of 13% from the previous year), but only 10% of specialty provider organizations have 20% or more of their total revenues in VBR contracts.
Use The OPEN MINDS Value-Based Reimbursement Readiness Assessment for analysis and recommendations regarding your organization’s VBR competencies. This tool was designed to evaluate and identify improvements in the following domains:
- Provider Network Management: Strategies to enhance provider networks.
- Clinical Management and Clinical Performance Optimization: Data analyzed to drive clinical decision-making.
- Consumer Access and Service Engagement: Processes to empower consumers and create engagement.
- Financial Management: Revenue cycle management and accounting procedures to support contracts.
- Technology and Reporting Infrastructure: Data leveraged to gain insight.
- Leadership and Governance: Alignment of strategy with infrastructure and resources.
The OPEN MINDS team will use these findings to determine the organization’s operational system capabilities for service delivery that meet health plan goals and performance expectations.
Development Of A Health Plan Partnership Concept Statement
With your health plan strategies and marketing objectives in place, along with the results from your VBR capabilities assessment, you can move onto the third component of Phase One: developing your Health Plan Partnership Concept Statement. Think of this as your initial “marketing pitch deck” for health plans. This Partnership Concept Statement is designed to introduce your organization to health plans and other payer organizations, highlighting your organization’s core competencies, core service lines, specialty programs, significant outcome metrics, reimbursement structures, and proposed areas of partnership.
It should be developed after an in-depth service line assessment to determine which of your organization’s programs and services are of interest to health plans and can be packaged and marketed for fee-for-service and alternative reimbursement health plan contracts. It should also affirm your value-based reimbursement readiness and unique organizational characteristics that would be of interest to health plans and their members.
Building The Health Plan Playbook: Identifying And Prioritizing Target Payers For Outreach
The next component is beginning the development of your “health plan playbooks,” a profile of an individual health plan along with details about your marketing tactics for the plan. Begin by identifying and analyzing payers (e.g., health plans, managed care organizations, managed behavioral health organizations, ACOs, and large employers) operating in your service area. The goal of the analysis is to prioritize the best targets for payer outreach based on the market factors that are driving payer network service needs and contracts with specialty provider organizations. I recommend developing an initial list of five payers for target market research.
Conducting Initial Health Plan Interviews
The fifth component is conducting initial interviews with the payers that you have selected in the preceding component. The goal of the interviews is to determine the service needs of each of the priority payers and identify contracting and partnership opportunities. Identify the “pain points” for each payer so you can determine how your organization can address them. Interview questions will focus on payer member service needs, population health management, service delivery gaps, underserved populations, provider network deficits, and contract opportunities. You will likely find that payers are looking for integrated physical and behavioral health care models, sophisticated virtual service delivery and marketing capabilities, care coordination approaches that follow the consumer across the continuum of care, data interoperability, and programs (either directly from you or through strategic community partnerships) to address the social determinants of health for the populations you serve.
Redefining & Implementing The Health Plan Playbook Strategy
With this deeper understanding of the priority health plan needs you’ve gained from the interviews, you should be able to revise your initial concept statement or marketing pitch deck for each payer. Additionally, it is here that you build out your playbook for each priority payer, including service line development, partnership opportunities, preferred contracting models, etc. Your health plan playbook strategy will include compiling program descriptions for the services you plan to pitch to each payer and should include leveraging evidence-based practices and program outcomes data for each service line. Pitching a VBR contract model, or a transition to one, will be attractive to health plan payers.
Health Plan Proposal Development
With all your homework, research, and insights handy, craft the proposal for each of your targeted health plans for the programs and services you are pitching. Include: any use of evidence-based practices, your infrastructure investments, consumer and community testimonials and endorsements, and demonstrated outcome measures.
Request a meeting (be sure to ask that administrative, as well as clinical leaders, from the health plan be in attendance) and present your proposal. Be sure to follow up after the presentation to see if anyone has questions or requires further details. Practice patience, but be sure to remain on each health plan’s radar by checking in frequently and letting them know you are still interested.
Contract Development & Negotiation
Once a health plan indicates that they are interested in your proposal and want to move forward, act quickly. See if there are opportunities to further negotiate rates and proposals based on market needs and the niche you can fill. There is always a win-win proposition; you can get there by offering options, making the effort to negotiate, and focusing on what you will deliver. Make sure the final contract goes through all the appropriate reviews on your end—legal, financial, clinical, and operational—before you sign and seal.
Implementing & Managing New Health Plan Contracts
The last component of the “Establishing the Right Set of Health Plan Contracts” phase is implementing and managing the new contracts you’ve won. Make certain that your key organizational systems are prepared to meet new contract requirements. These functions include:
- Intake/admissions/authorization processes
- Care management
- Referral development optimization
- Service delivery process enhancement
- Performance reporting for teams and health plans
- Contract management systems
Designate an account manager who will nurture the health plan relationship, serve as a key liaison between the health plan and your team, monitor how the contract implementation is going, facilitate dialogue if there are issues to be resolved, and ensure that all parties are satisfied. Develop marketing and referral development strategies to get new referrals flowing and implement performance monitoring and improvement mechanisms. Monitor performance continuously to ensure that you are building customer satisfaction to maintain and grow your partnership with them.
With the right set of contracts established and implemented, the next phase in the three-phase framework for sustainable health plan relationships is about how to optimize your contracts and implement formal contract management operations.
