By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Every organization in the health and human service system field is developing strategies to optimize their ability to participate in whole person care and population health initiatives, which will maximize consumer care and outcomes, as well as improve payer relationships both today and tomorrow. This includes planning for integrated care delivery, hybrid service delivery, and performance-based reimbursement models.
For large health systems, the mandate for whole person care presents several challenges. These include integration of their own service delivery system with external providers organizations and care coordination across disparate locations and levels of care. But market forces are driving hospital executive teams to rethink their strategies. Nearly 9 in 10 emergency physicians reported that psychiatric patients were being held in their emergency departments for hours and days. And while only one-third of community general hospitals have inpatient psychiatric units, more than 2 million discharges from community hospitals were for a primary diagnosis of mental illness or substance abuse disorder.

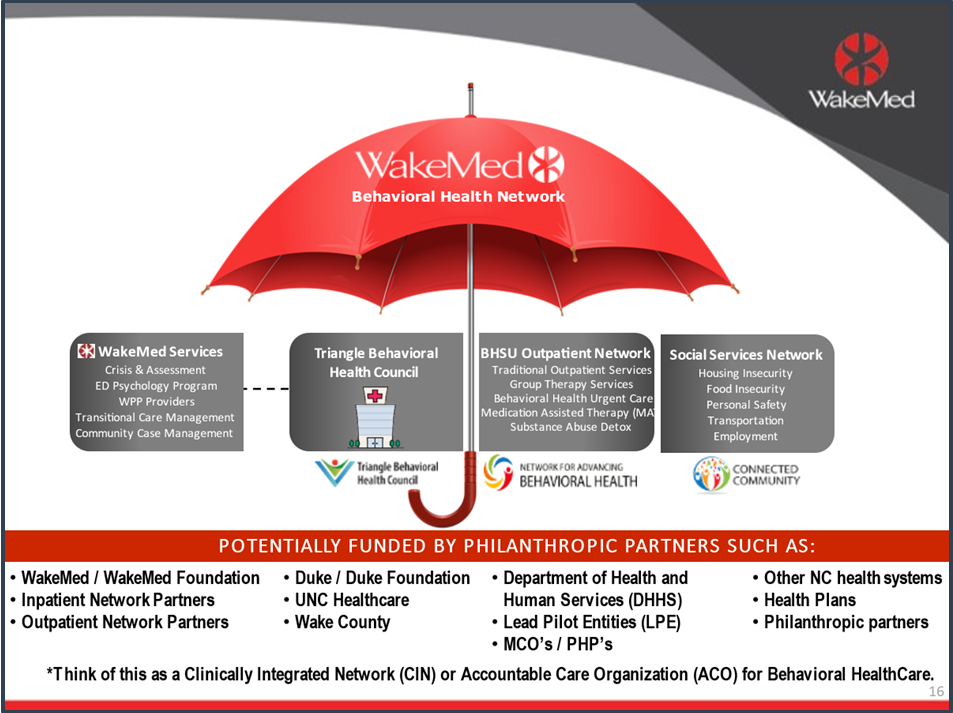
One hospital, WakeMed Health & Hospitals (WakeMed), has created an innovative approach to meeting the whole person care needs of their community. They employ a model that integrates their delivery system capabilities (psychiatry and inpatient psychiatric services, and primary care) with a behavioral health outpatient network, inpatient network and a social services network that form the WakeMed Behavioral Health Network (WMBHN). This innovative model is the focus of Rick Shrum’s keynote, “WakeMed’s Path to a Population Health Model for Behavioral Health: The Development of the WakeMed Behavioral Health Network”, at The 2023 OPEN MINDS Performance Management Institute in Clearwater Beach, Florida. Mr. Shrum is Vice President and Chief Strategy Officer for WakeMed Health & Hospitals based in Raleigh, North Carolina.
The needs of the community that WakeMed serves drove this innovative approach to behavioral health care. In 2017, WakeMed responded to more than 40,000 encounters across seven emergency departments (EDs) for substance use and psychiatric disorders. However, their behavioral health service was not integrated enough with other community providers, which slowed delivery of treatment and services. Annually, there are approximately a total of 300,000 visits to their seven emergency departments. Before the pandemic that included 35,000 to 40,000 people with behavioral health conditions, but that number has grown to 50,000 to 60,000, a 30% increase (inclusive of a 66% increase in child/adolescent ED presentations). Even more alarming is the increase in the severity of illness evidenced by a 35% increase in suicidal ideation, and a 68% increase in overdose.
Addressing these needs was the driver of the formation of the WMBHN. To improve integration, WMBHN created a shared electronic health referral system so clinicians can perform behavioral health and social determinant screening to determine which services are necessary, and then electronically match and refer to providers that are right for the consumer’s health care needs. In addition, they developed a proprietary patient severity-of-illness tiering tool to assess overall illness level. WMBHN includes three sub-networks with providers who focus on inpatient, outpatient, and social determinants of health that all form a unique, community-wide approach to address growing behavioral health needs. There are currently 37 participating organizations in WMBHN representing over 2,500 behavioral health clinicians statewide.
According to Mr. Shrum, success for WMBHN was based on four pillars: use of common screening tools, mitigation of social and medical obstacles, application of best-practice, patient engagement techniques, and coordination at all levels of follow-up care. As a result, the network dropped referrals to statewide hospital beds by 87%; improved access to outpatient services, including first-time patient show rates from 20% to 85%; decreased the 30- to 60-day readmission rate by 27%; and decreased involuntary commitments by 30%. Perhaps most importantly, consumers receive treatment 72% faster than before creation of WMBHN.
Mr. Shrum recognizes how those results tie back to the population health concept. “Behavioral health is siloed in most communities, and individual organizations, health systems included, cannot do this important work alone, it literally takes a village!” he said. “Health systems are uniquely positioned to help lead a new way forward in population health. And there is such strength in the collective as it applies to most communities’ number one health challenge – behavioral health care.”
