By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Social service programs will soon play a new role in the health care system. Earlier this year, CMS changed the rules for Medicaid health plans, allowing them to spend health care premiums on social service programs. CMS also recently approved the State of California’s proposal to provide Medicaid services in corrections facilities. And fourteen other states have applied to CMS for similar Medicaid corrections in-reach service waivers.
These changes will increase the spending on services for health care-related housing, transportation, and food services. But bigger spending will increase the health plan demands for more rigor in defining best practices, in determining eligibility for services, and in models for performance measurement and reimbursement. We got some perspectives on the current state of “best practices” in these programs in a session, Addressing Social Determinants Of Health To Achieve Whole Person Outcomes, at The 2023 OPEN MINDS Performance Management Institute. The session featured Charles Gagnon, Chief Executive Officer, and Mindy Miller, Chief Operating Officer of Volunteers of America of Massachusetts (VOAMASS), Jorge Petit, M.D., President and Chief Executive Officer for Services for the UnderServed, and Janikaa Sherrod, Associate Vice President of VOA Health and VOA Justice for VOA Mid-States.
VOAMASS serves thousands of families across Massachusetts, providing services for chronic challenges facing its communities including illicit opioid use, mental health, housing, unemployment, elder care, and recidivism among justice-involved residents. New York City-based Services for the UnderServed provides services for transforming the lives of people with disabilities, those in poverty, and those facing homelessness. VOA Mid-States in Louisville, Kentucky, one of the region’s oldest not-for-profit organizations, reaches people through nearly 50 programs across four states through addiction recovery, developmental disability, health, homeless/housing, restorative justice, and veteran services.
The faculty presented three case studies of innovative approaches to meeting consumer social service needs. A common theme of each was the importance of a standardization of the assessment of consumer needs and a collaborative care team.


The panelist spoke to the importance of standardizing needs assessments for each consumer. VOAMASS uses one centralized comprehensive assessment for social determinants of health (SDOH) needs—using the Protocol for Responding to & Assessing Patients’ Assets, Risks & Experiences (PRAPARE). This assessment, conducted by a licensed behavioral health professional, allows them to identify health-related social needs leading to a more comprehensive care plan. But there are a number of validated tools that are available to use in an assessment of consumer SDOH needs.
“We ask social determinants of health questions. We didn’t do that before on behavioral health, which is crazy to think now that we know how important it is,” said Ms. Miller. “We started to ask more questions to really understand the whole person perspective.”

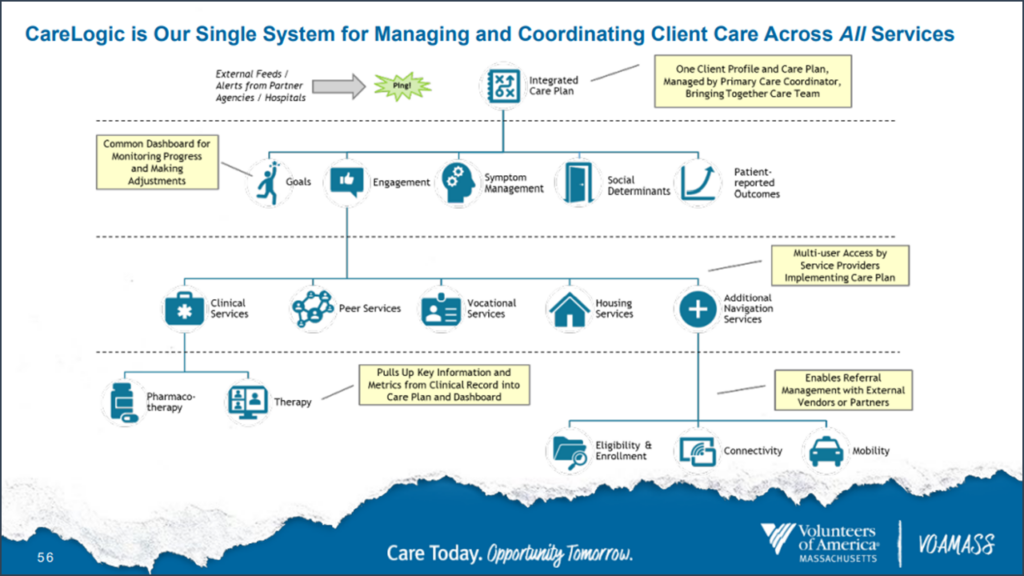
Using that data, collaborative care coordination is also an essential ingredient. And the right technology is critical to making that happen—facilitating sharing data across the health and human service system, including payers and as community partners. The right platform allows all parties access to consumer assessment data to develop consumer goals and the right care plan. The platform also facilitates care coordination between clinicians, coaches, caregivers, health and social service organizations, and community organizations, a key to assuring continuity of services, facilitating referrals and reducing redundancy. And coordinating data collection allows performance measurement on an individual consumer and aggregate basis.
When it comes to care planning, Ms. Sherrod from VOA Mid-States said her organization takes a “targeted universalism” approach to making healthier communities. Under this strategy, universal goals are set for everyone within targeted populations to help specific groups. “It helps us tailor to each population the goal that we need them to reach so that we don’t leave out any individuals or groups of people that we serve,” Ms. Sherrod added. “That is how we design and implement our services at VOA Mid-States.”

Services for the UnderServed, which operates in all five boroughs of New York City and on Long Island, has made collaboration the linchpin of its myriad of service offerings including behavioral health services, intellectual/developmental disabilities services, homeless services, treatment services, and veterans’ services. The organization’s collaborative care teams provide “the gamut of services on a continuum—everything from outreach teams, ACT teams, crisis respite, clinic services, clubhouse, and employment opportunities,” said Dr. Petit. “It’s all about social justice and really figuring out ways for us to engage around actions that are much more intentional and directed.” He said the goal is to create “an integrated, holistic one-stop shop No Wrong Door.”
To move to whole person care models that span behavioral, medical, and social needs, organizations need to assess the functionality of their current consumer care platforms and its utility in care management. And, despite some barriers with data sharing, implementing cross-organization consent to support an “opt-out” rather than the dated “opt-in” approach is one way to transcend data-sharing barriers.
The past decade has seen a change in payer and health plan interest in the effects of social conditions on health care utilization—and initial efforts to develop models that address those needs with a measurable outcome. The challenge ahead is building on these initial efforts and taking these models to scale. That work appears to be underway. In North Carolina, the state has developed a menu of social services with fixed criteria and prices. This was discussed by Elizabeth Cuervo Tilson, M.D., MPH, State Health Director and Chief Medical Officer for North Carolina Department of Health and Human Services, in her presentation Connecting The Dots: How North Carolina Is Creating A Statewide Coordinated Network For Whole Person Health at The 2022 OPEN MINDS Technology & Analytics Institute.
There are some interesting new initiatives at Humana. Stephanie Franklin, the Director of Population Health for Humana, shared their approaches in What, When & How To Share Data – Innovating For Social Needs & Population Health Strategies at The 2022 OPEN MINDS Technology & Analytics Institute. And Abbie Gilbert, Associate Director, Office of Health Affairs & Advocacy with Humana, with Stephen Samuels, Vice President, Innovation and Impact Investing for Volunteers of America, presented a collaborative model for delivering social supports in their OPEN MINDS Circle Executive Roundtable, Fostering Innovation & Entrepreneurship With Managed Care Organizations — The VOA & Humana Case Study.
Whatever becomes the accepted “best practices” it is likely that the integration of social services in the health care continuum is going to have the same rocky trajectory as the integration of behavioral health and primary care. And in that change is opportunity.
