By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Patient engagement, motivating consumers to choose to participate in their own care, was top of mind in the health and human service field this year if the number of professional meetings focused on the topic is any indication. There was the National Health Council’s 2023 Science Of Patient Engagement Symposium and the Patient-Centered Outcomes Research Institute’s Advisory Panel on Patient Engagement Fall 2023 Meeting, to name just a couple.
The reason for that focus is clear. Without patient engagement, many investments in evidence-based practices, new workflow processes, and new technologies have limited impact. A meta-analysis of patient engagement outcomes, published as Impact Of Patient Engagement On Healthcare Quality: A Scoping Review, found four main areas of impact for patient engagement programs—health outcomes, patient adherence, consumer self-direction, and financial returns. Interestingly, there are studies on the impact of patient engagement on the three areas of impact, formal studies of the financial returns of investments in patient engagement are more limited.
A few months ago, at the 2023 OPEN MINDS Executive Leadership Retreat, we got a first-hand look at the impact of a patient engagement initiative at a behavioral health provider organization—COPA Health. The session, sponsored by NextGen Healthcare, What If You Build It & No One Comes: Patient Engagement In Whole Person Care & Value Based Payment, was led by Dr. Michael Franczak, Director of Population Health at COPA Health and my colleague, Christy Dye, Senior Associate at OPEN MINDS. COPA Health is a non-profit provider organization based in Arizona that provides educational, therapeutic, rehabilitative, and social services to children and adults with developmental, physical, and behavioral health challenges across the state. The organization has annual revenue of over $71 million.
COPA’s interest in patient engagement initiatives was initially triggered by high ‘no show’ rates—nearly 25%—causing clinicians and the organization to lose valuable productive time and compromising consumer outcomes. As clinicians and case managers were booking appointments, no shows were taking large blocks of time from their schedules with no room to bring a new patient in for services quickly.
Dr. Franczak and his team launched a pilot program focused on reducing those high ‘no show’ rates. The first step was analyzing two years of data. To optimize this analysis of the data, they deployed artificial intelligence (AI) tools. “I embrace AI because it’s bigger…than a database. We have a great database, a great data warehouse, where we import all kinds of data from our HIE, from our software, from our EMR. We then apply algorithms and statistical analysis to the data,” said Dr. Fanczak. “Artificial intelligence can tell us the who, what, when, and where but not the why. That’s where the clinical team are able to identify the specific causes for each individuals engagement or lack thereof.”
The resulting data analysis showed multiple causes for no show appointments. First, schedulers had no insight into the consumers’ previous no show rates which would have allowed them to proactively provide more supports—reminders, check-ins, etc. They also found that COPA’s scheduling processes were inflexible and didn’t include consumer input. The data also showed that housing instability and transportation issues were causes of many no show appointments.
The pilot program also revealed some internal workflow issues leading to some staff needing to be retrained. On-boarding and trainings of staff were inconsistent across the clinics and needed to be updated and standardized to implement the new information that COPA had. Staff had to be re-trained on how to best utilize telehealth technologies and not to rely on scheduling software and automated reminders to be the only points of contact for the consumer.
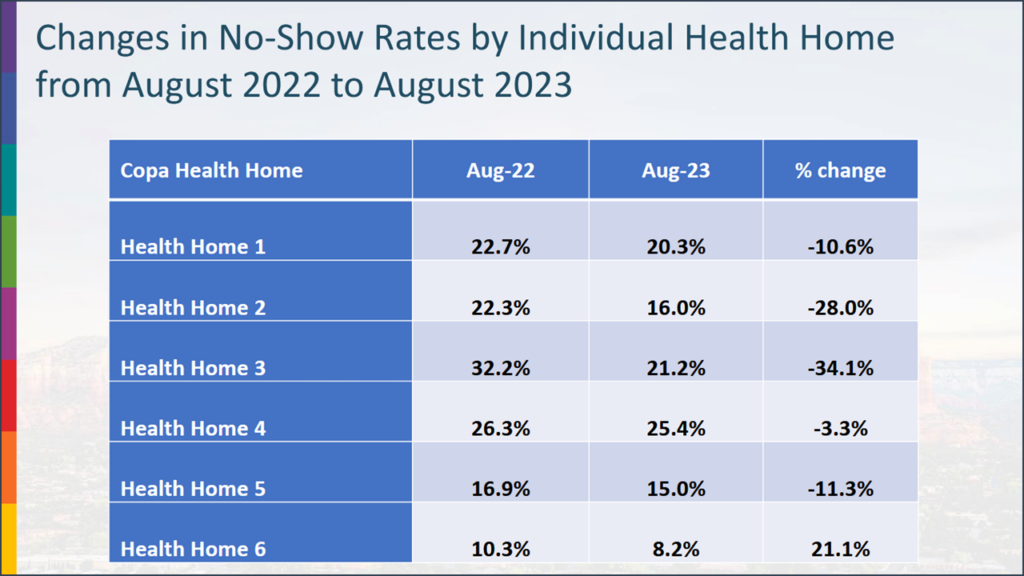
Over the course of just 6 months, Dr. Franczak and his team were able to reduce no shows by 50% in their West Valley Clinic. Over the course of a year, they were able to drop no show rates in their East Valley clinic from 25% to 12%. And the COPA team continued this initiative across all of their locations. “Once our clinicians can see patterns of no shows and dropouts from our AI database, they are able to use that information, turning it into actionable intelligence focused on the root causes of the problem,” shared Dr. Franczak.
Reflecting on the COPA case study, Ms. Dye commented, “Access, appointment participation, and follow-through are key elements to successful patient engagement.” Rapid access to appointments keeps consumers engaged and more likely to show for the appointment. “You want to get people in fast, right? So when they make contact, however they make it, they can rapidly get access to an appointment,” said Ms. Dye.
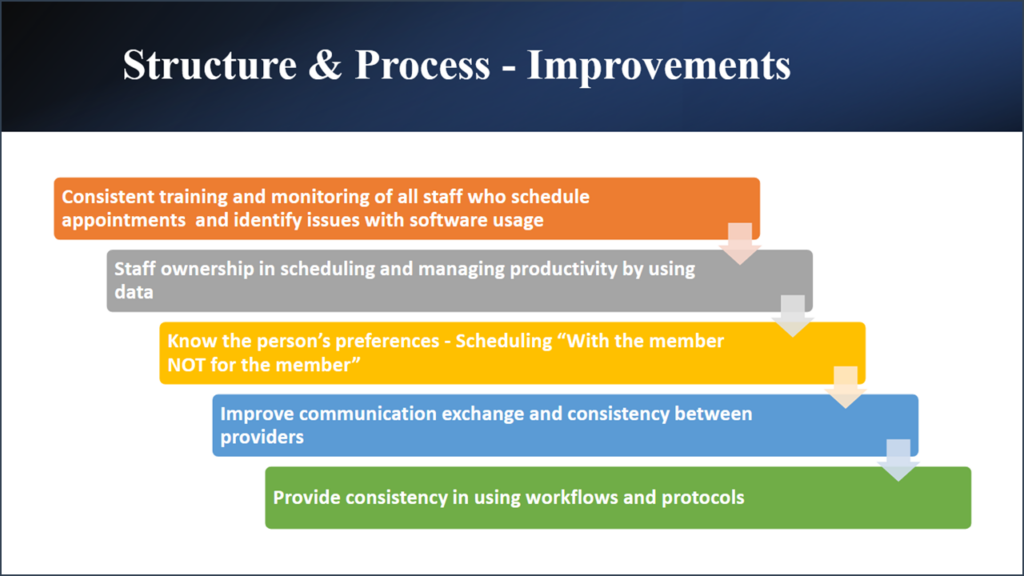
She continued, “Appointment participation is a key measure of engagement—and important to maintaining engagement, reducing no shows, and sustaining clinical productivity…Care gaps are hard to close. It’s even harder to close if the person doesn’t show up.”
Ms. Dye also observed that follow-through with consumers as part of on-going care coordination is another essential element in patient engagement. “Fewer than 50% of people have seen their mental health practitioner within seven days of discharge from a hospital after harming themselves,” Ms. Dye shared. “This is an incredibly vulnerable time for consumers in that situation and acts as just one example where care coordination and follow-ups can make a big impact.”
As clinical outcomes, consumer experience, and cost become more important to competitive advantage, patient engagement strategies will become more central to success. Executive teams will need to think through the processes and the technology needed to make that happen. But it often seems like an overwhelming task. To that Dr. Franczak had some advice: “You’ll want to take a big audacious goal and break it down into smaller measurable goals.”
