By Monica E. Oss, Chief Executive Officer, OPEN MINDS
Clinical decision support (CDS) tools are getting more attention this past month. There is the report of “72% accuracy” of ChatGPT in clinical decision making. AI-infused chatbots are seen as an emerging clinical decision support tool. Plus, just two weeks ago, the Department of Health & Human Services released new rules called Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency and Information Sharing known as HTI-1 requiring transparency in the algorithms used for clinical decision making.
While using CDS tools is just one of many strategies to improve quality and consistency across the health and human service care continuum, it is becoming an increasingly important one. On the payer side of the equation, CDS tools assist a health plan’s speedy dissemination of best practices across its network of provider organizations. On the provider organization side of the equation, CDS tools are a partial solution to the care quality issues created by high turnover among clinical staff. If CDS platforms are so important, how are they being implemented and employed by executive teams and their organizations?

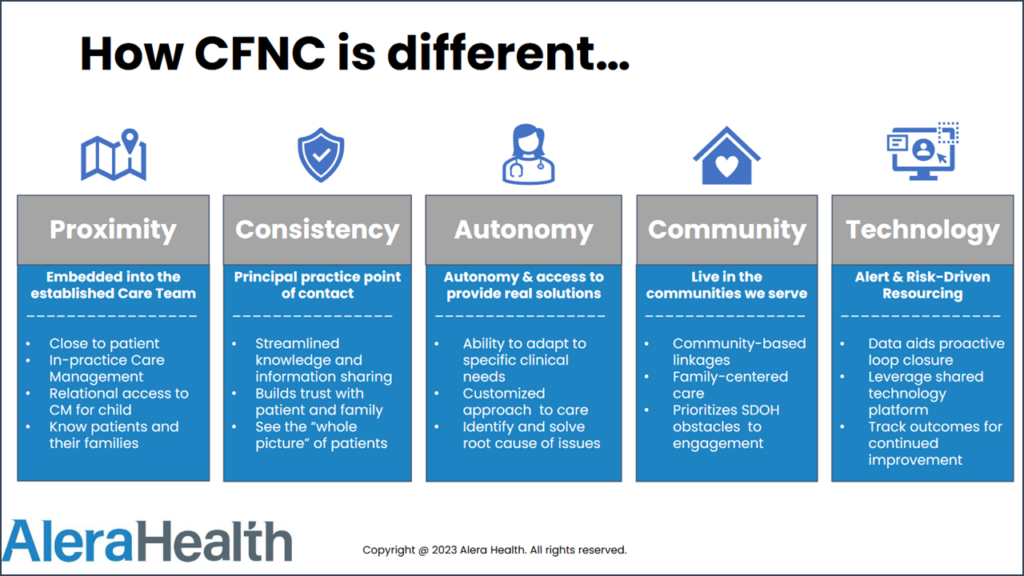
Addressing that challenge was the focus of the recent session, Removing Noise From The Signal: The Data Is Speaking, Are You Listening?, at the 2023 OPEN MINDS Technology & Analytics Institute. The session featured Zach Strong, FNP-C, a family nurse practitioner at Salisbury Pediatric Associates and associate director of care management at Children for First North Carolina (CFNC) along with Jose Castillo, MBP, PMP, senior vice president of health informatics, and Mary Ann Crowder, Ed.D, executive director of information technology program development, with Alera Health.
The panelists walked through their process of designing a clinical decision support system for CFNC and highlighted how CNFC staff utilized the platform to deliver quality outcomes in preparation for the shift to value-base care.
CFNC is a clinically integrated network of two pediatric practices with five locations in North Carolina that serve 18 North Carolina counties and provides care management to over 35,000 children and their families. The organization is a member of one of Alera’s ONEcare Networks, integrated systems of care for patients with primary and secondary behavioral health issues. The panelists highlighted the key steps in developing a best practice CDS system—identifying data sources and confirming their quality and consistency; developing algorithms for analyzing the data and identifying thresholds for clinical action; and designing the system for pushing information to the clinical team.
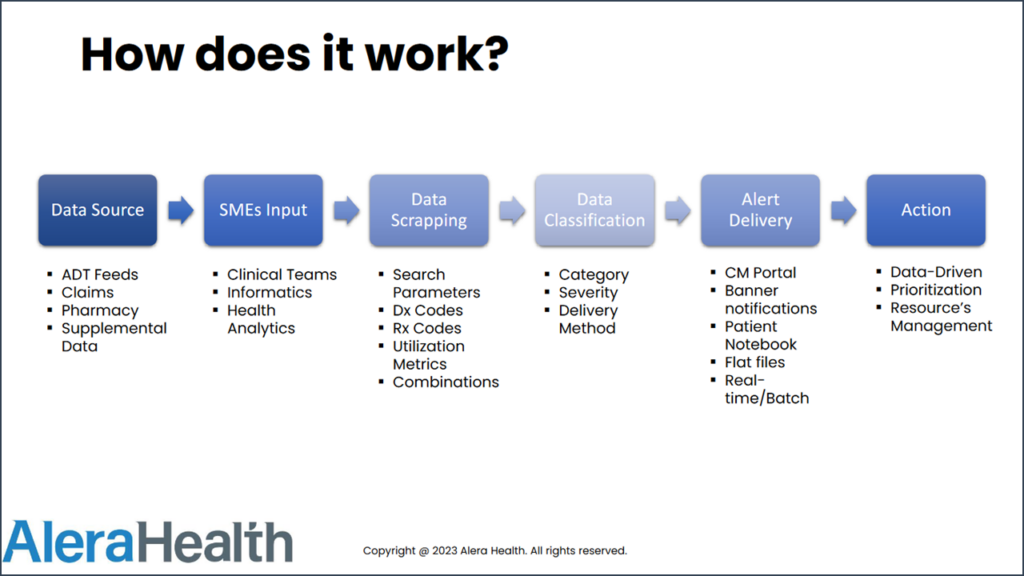
Identifying data sources and confirming their quality and consistency. The first hurdle is the fact that consumer data likely comes from numerous sources and will contain abundant data points—diagnoses, prescription recommendations, assessments, claims data, utilization patterns, and more. The first step of building a CDS function begins with a review of all available data—and its quality.
In building a CDS function for CFNC, the Alera team started with North Carolina’s local health information exchange (HIE)—and worked with the CFNC clinical team to narrow down the full dataset to just the data elements essential to care coordination. “It’s not just about the source, but the quality and consistency and availability of that information…to make the sure the feed is not only useful, but reliable and consistent over time,” said Mr. Castillo.
Developing algorithms for analyzing the data and identifying thresholds for clinical action. The next step in the CDS development process is creating the rules and criteria for using the data in clinical decision making. Generally, these rules should be built around specific use cases in the organization—like early intervention for consumers with deteriorating health status or assuring adherence with medication regimes. The use cases provide a framework for the criteria that drives action from the clinical team.
The speakers discussed one such use case—improving outcomes for consumers that use inhalers to manage their asthma. The CFNC team was interested in identifying consumers who were overusing inhalers, indicating that their asthma was not being well managed. CFNC created an alert related to the number of refills of inhalers in a month—triggering outreach from the clinical team for a reassessment. “If you have a patient that is refilling their rescue inhaler two [or] three times a month…that likely means their asthma is not well managed…and we need to get to the bottom of what is going on,” Mr. Strong shared.
Designing the system for pushing information to the clinical team. The final step in using a CDS system is designing how the information will be communicated to the clinical team in order to drive action. There are a wide range of options—from email and text alerts to a clinician related to a specific consumer, to clinician-specific and consumer-specific call outs in EHR systems, to special notices in care coordination/population health management dashboards. The key is to make these calls to action part of the clinicians’ standard workflows and easy to understand. CFNC embedded those alerts in the Alera platform used by clinicians on a regular basis.
“The idea is to distill meaningful information to [clinicians] to do what they do best,” said Mr. Castillo. The CFNC dashboards include patient name, the alert message, the alert category (for example whether it was a clinical alert or a pharmacy alert), date that the alert was delivered, and the alert severity. The alerts must also get to the right staff member. Having the right data and the right alert go to the “The idea is to distill meaningful information to [clinicians] to do what they do best,” said Mr. Castillo. The CFNC dashboards include patient name, the alert message, the alert category (for example whether it was a clinical alert or a pharmacy alert), date that the alert was delivered, and the alert severity. The alerts must also get to the right staff member. Having the right data and the right alert go to the wrong clinician negates any benefit and CFNC made sure that as the data was pulled and the alerts were created, the right clinicians were assigned to the right notifications. “Making sure the right person is addressing the right need is going to provide better care,” stressed Mr. Strong.
With the rate of new medical developments increasing faster than the ability of provider organization clinical teams to assimilate and apply it effectively, the need for just-in-time actionable information for consumer care coordination is only going to increase. The question for executives in the health and human service field: how to lead and manage in a time when knowledge becomes quickly outdated and replaced by something new? One of the answers is to imbed clinical decision support in the service delivery continuum.
