By Monica E. Oss, Chief Executive Officer, OPEN MINDS
The collaborative care model (CoCM) is an important part of the move to whole person care in the health and human service system. Defined as a model that “leverages the coordinated efforts of a primary care or specialty medical care provider (PCP or SCP), a behavioral health care manager, and a psychiatric consultant, using a structured, measurement-based framework,” a recent study—Trends In Adoption Of The Collaborative Care Model—found that the adoption of CoCM has significantly expanded across all major insurance coverage types since the introduction of dedicated billing codes (and associated payments) in 2018. This includes Medicare (where CoCM is fully covered), the commercial market (where CoCM is widely but not universally covered), as well as Medicaid and the Children’s Health Insurance Plan (CHIP), where some states have activated the CoCM codes.
The proportion of individuals receiving collaborative care services increased from 10.0 to 56.1 individuals per 100,000 in Medicare from 2018 to 2022. In the commercial market, this increase went from 2.2 to 58.8 individuals per 100,000, respectively, in the same period.
Participation in CoCM varies widely by geographic market. The markets with the highest use of the model include Madison, Wisconsin; Jackson, Michigan; Bellingham, Washington; Albany-Lebanon, Oregon; Corvallis, Oregon; and Prescott Valley-Prescott, Arizona.

With the expansion of whole person care models, most provider organization executives are rethinking their strategies for participating in integrated care. We had a look at how one organization has expanded its service offerings to embrace whole person care in the recent OPEN MINDS Executive Roundtable, Strategies For Hybrid Care For Diverse Populations, The MyCHN Case Study. The MyCHN leadership team of Yvette Poindexter, M.D., Chief Medical and Operations Officer; Penny Pabst, Chief Administrative Officer; and Nydia Garcia, Quality Director, presented their advanced integrated care model.
Based in Greater Houston, Texas, MyCHN is a $123 million provider organization that is both a federally qualified health center (FQHC) and a certified community behavioral health clinic (CCBHC). In just over 15 years, it has expanded to serve nearly 50,000 consumers annually. It operates 20 permanent clinics, three mobile clinics, and multiple pharmacies across three counties.
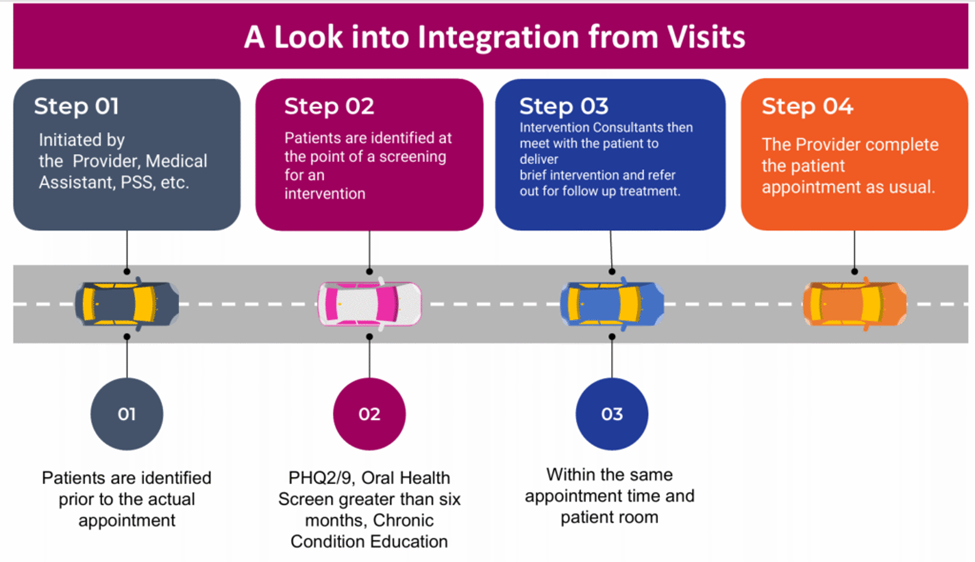
MyCHN’s model is patient-centered and integrates primary care, specialty care, behavioral health, pharmacy, and dental care. Support services include case management, non-medical drivers of health, eligibility verification, chronic care management, patient navigation, at-home health care, crisis services, and peer support. Once consumers are screened by MyCHN’s primary care clinicians, they receive referrals to specialty services for either those provided internally by MyCHN or external referrals based on geographic location and insurance coverage.
These services are delivered in the Texas counties of Brazoria, Harris, and Galveston. MyCHN’s payer mix for this model includes Medicaid/CHIP (36.9%), private insurance (27.4%), self-pay (26.2%), Medicare/Medicare Advantage (6.3%), and grants (3.2%).
The outcomes from the integrated care model are impressive. In 2024, half (50.3%) of MyCHN’s consumers with behavioral health conditions received integrated services. In the same year, 1.54% of the consumers participating in these services were hospitalized. From December 2023 to November 2024, the percentage of consumers aged 12 and older in the program who had a remission in major depression or dysthymia was 66%. (This exceeds the national benchmark of 14% and the Texas state benchmark of 20%.) MyCHN also reported that consumers had improvements in diabetes and hypertension management and an increase in depression screening. Consumers receiving integrated care also reported fewer suicidal ideations, improved mood stabilization, better coping strategies, and higher levels of engagement.
For executives considering an expansion into this type of model, the MyCHN team had some advice. They advised executives to focus on building a whole person “ecosystem,” leveraging technology for better consumer access, and measuring and monitoring more than clinical outcomes.
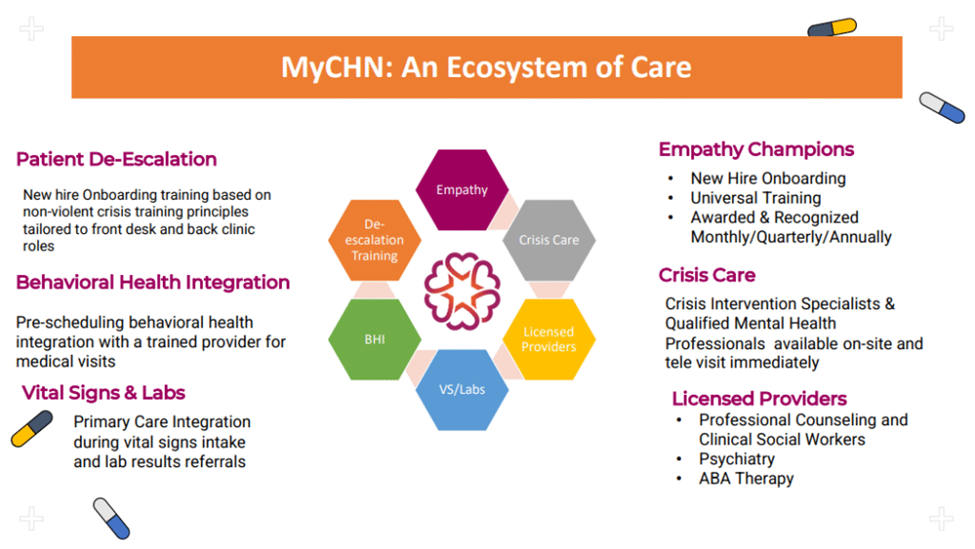
A fundamental of moving to an integrated model is creating what the MyCHN team calls “an ecosystem of care” that starts with embedding this approach into organizational culture with “no wrong door” access and approaching consumers as a “whole person” from the first contact. “Our culture starts with our CEO, through different protocols and different teams that were designed to build out the services that transformed the organization,” Ms. Garcia said.
On the technology front, the MyCHN team expanded their hybrid telehealth care and remote monitoring capabilities to better manage chronic conditions and improve consumer convenience. They focused on rapid access to prevent consumer health conditions from worsening and to build trust among consumers who might otherwise disengage from care.
“Technology and various types of hybrid virtual visits provide continuous access to care across our ecosystem,” said Ms. Garcia. “We’re always looking to see how we can provide care across all services.”
And finally, while clinical metrics are important, the MyCHN executives recommend tracking additional outcomes like consumer empowerment, quality of life, and consumer engagement, which are increasingly important to success in providing whole person care. These “human-centered” measurements demonstrate additional aspects of the value the organization delivers to consumers, and these metrics enable executives to bring additional data demonstrating value to payer negotiations and contracts.
They note that in a whole person approach, lab values and outcomes tell part of the consumer’s story, but the narrative of their progress through their care journey has other pieces, too. “When the person is engaged and empowered, they are actively involved with their care team, resilient, and embracing healthier coping strategies,” Ms. Garcia said.
The MyCHN team was very positive about their whole person care model— for their organization and the consumers they serve. “I always believe in starting where you are,” said Dr. Poindexter. “What service do you already have? If you have behavioral health services, what other services do you have on-site? Do you have access to outsource any type of chronic care management services that would serve as an integrated care model? It all depends on where you start from.”
