Consumers want a convenient experience, and payers want value for health care expenditures. Both of these stakeholders are looking for these qualities in whole person care models.
Topping the consumer ‘wish list’ for health care is a convenient experience, with ready access to services and low costs. For executives provider organizations (and health plans), making this happen has been a challenge.
For payers and health plans, the interest in integrated care delivery using whole person models is driven by cost factors. In the U.S., 10% of consumers use 70% of health care resources. And half of those consumers have a behavioral health disorder, cognitive disability, or a neurological condition. The key to better health outcomes and lower costs is an integrated care coordination model.
Initial studies of integrated care models are positive. Studies find improved consumer experience, improved health status and clinical outcomes, and reduction in total cost. And the initial ROI data for integrated care pans out, particularly integrated care arrangements with downside financial risk arrangements with provider organizations.
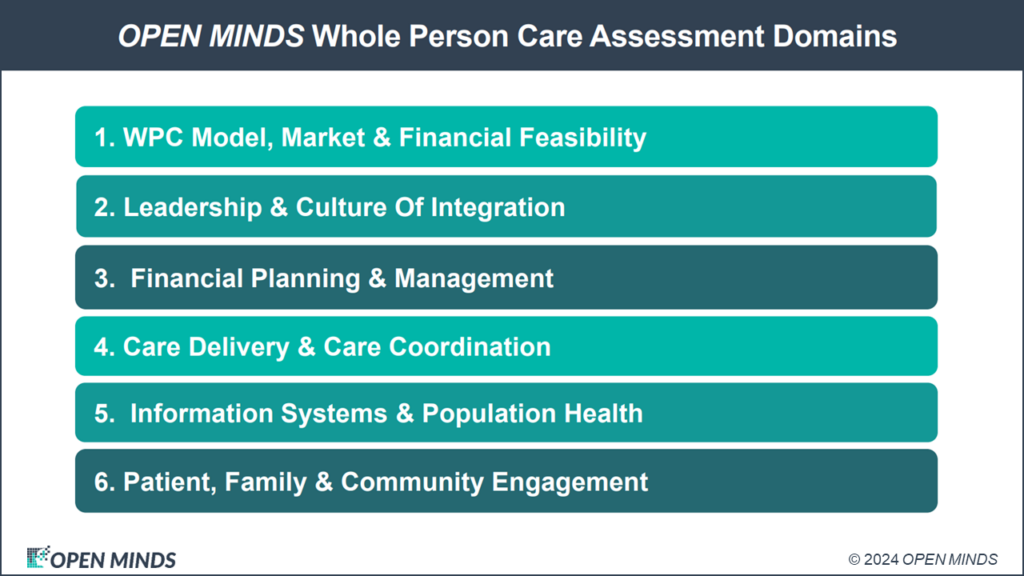
The question for most provider organizations is how to participate in integrated delivery systems. While Certified Community Behavioral Health Clinics (CCBHCs) are a strong contender as the most-preferred model in mental health and addictions, there are dozens of approaches to combining hybrid, virtual, and in-person services in varied delivery settings based on population needs, local market factors, and provider capacity. The issue of selecting, and improving, integrated care model performance was the focus of our recent OPEN MINDS Executive Roundtable, How To Improve The Performance Of Your Existing Whole Person Care: Assessing Your Program Positioning, featuring my colleagues OPEN MINDS Senior Associates Deanne Cornette and Christy Dye. Their approach to selecting and improving those models was focused in four key areas—build a financially viable business model, focus on consumers with complex needs, invest in technology, and create deliberate models for collaboration with other payer and provider organizations.
The financially viable business model The first issue is selecting the right integrated care model—one that is financially sustainable. The ‘right’ model will depend on the consumers served and the health plans that provide their coverage. At a minimum, models that focus on ‘virtual care coordination’ require data sharing and interoperability. At the other end of the spectrum, provider organizations can deliver the full range of services—medical, behavioral, and social—through their own staff or their own network model. Whatever the model, the costs of coordinating services across systems are significant—a recent analysis put the cost of social care coordination at $60 per person per month.
Most executive teams only build operational budgets to estimate the infrastructure and ongoing costs of delivering integrated care. Better performance, however, means devoting time and energy to testing the financial feasibility of the model. A solid business plan aligns payment rates, payment models, the anticipated volume of consumers, and staff productivity. Doing this successfully means using a three-year forecast to first reach “break even” and then earn the necessary positive margins.
“The financial proforma is what allows you to test financial scenarios as you ramp up your whole person care services,” said Ms. Dye. “If I have a three-year proforma, how long will it take me to break even? How long will it take to reach an acceptable rate of return and margin? And what losses might I incur?”

Focus on consumers with complex needs For most provider organizations, whole person care models have a better return (and better market advantage) if they focus on high-needs consumers. Those consumers with behavioral/cognitive conditions and physical health problems are an unserved population in most market..
Building a dedicated team to focus on clinical strategies and interventions for these consumers can make a big impact on their total cost by diverting them away from emergency departments (ED) and frequent hospitalizations. The upshot is an improved relationship with payers and potential bonus payments for reducing high-cost utilization.
“Organizations need dedicated staff or technology solutions to manage the complex care population,” said Ms. Dye. “We know for instance that the 30 days following a hospital discharge is a high-risk time and assigning care coordinators to follow up with the person to verify they understand their medications, have support systems in place and address fears and concerns can make a big difference in reducing re-admissions.”Provider organizations can also use technology tools for remote monitoring of the home to make sure environmental systems like lights and air conditioning are functioning or send staff out to assess conditions in person. “I live in the Arizona desert,” Ms. Dye said, “And a broken air conditioner in July meant multiple trips to the emergency room for our complex consumers. We saved the health plan lots of money by fixing that air conditioner.”
Invest in technology Technology is a “must-have” investment for participating in integrated delivery systems and offering whole person care services. Data sharing and interoperability for care coordination are fundamental to all of the models. But to be cost effective, provider organizations also need tools to support measurement-based care and HEDIS tracking, consumer engagement platforms, and population health tools for risk scoring and identifying care gaps and high-cost patients. Telehealth capacity using pads or smart phones can support delivering services in the home and community, while a mobile documentation or Ai-powered ambient note system enables those staff to capture all of their services for billing while they are still in the field.
At a minimum, provider organizations will need an electronic health record where all disciplines can contribute to a shared care plan. Ideally that EHR can consume external data feeds so staff do not spend time and energy on manually hunting down the latest lab test result or notes from an outside specialist.
“Access to external data allows the organization to be on top of key events, ideally in real time as they are happening,” said Ms. Dye. “A great example is a real-time notice when an individual is discharged from a hospital. A very common behavioral health HEDIS measure is to follow up to a hospital discharge within 7 or 30 days, but it is very difficult to do if you don’t know when the discharge actually occurred.”
Create deliberate collaboration models Regardless of the model and the size of the provider organization, collaboration with other provider organizations, social service organizations, and payers is essential for making whole person care models work. The key is to design deliberate models for collaboration—what provider, communication process, and more.
“Organizations need to provide opportunities for professionals from diverse backgrounds to collaborate on creating individualized care plans,” said Ms. Cornette. “Interdisciplinary approaches ensure a thorough consideration of a consumer’s physical, mental, emotional, and social health.”
Whole person care models are growing in importance in the field—in every payer group. Medicare Advantage plans are taking a whole person care approach with their Medicare populations and providing a wide range of social services. For more on Humana’s approach, check out the presentation, What, When & How To Share Data – Innovating For Social Needs & Population Health Strategies, by Stephanie Franklin, MPS, Director of Population Health for Humana.
Medicaid plans are moving to whole person care through two separate types of initiatives. There are ‘vertical’ health plans providing the full range of medical/behavioral/social services for specific types of consumers. And Medicaid plans are also paying for a wide range of social services, due to the new policy rules. Even employers are enhancing their plans with new integrated care models.
And there is more payer push for these models ahead. In January, the Centers for Medicare & Medicaid Services (CMS) announced a new integrated behavioral health (IBH) model in eight states and before July CMS expects to announce up to 10 new states entering the Certified Community Behavioral Health Clinics Section 223 Medicaid Demonstration Program. For most provider organization executive teams, the many possibilities are overwhelming. The challenge (and the opportunity) is to design a whole person care approach that is a best fit in their market.
