The Olmstead Decision turned 25 this past June 22. The promise of this landmark decision was to move people with disabilities into community settings, and it has had an impact. For consumers with I/DD, the number living in large, state-run facilities has dropped from nearly 200,000 in the 1960s to below 20,000 today.
But the waiting lists for home- and community-based services remains. About 692,000 people were on waiting lists or interest lists in 2023, and a majority of consumers on such lists have I/DD.
Consumers with I/DD make up 88% of waiting lists in states that do not screen for waiver eligibility. By comparison, consumers with I/DD make up 51% of wait lists within states that screen for waiver eligibility before adding individuals to the wait list.
These initiatives have brought a new focus on performance to the I/DD services delivery system. The most common performance measures in the I/DD systems include employment, access to care, and individual experience data reporting on their level of self-determination.
It is likely that the move toward managed care models for the I/DD system will continue and expand. And we had a focused look at how provider organization can best prepare for this continued transition in the session, Regulatory & Funding Changes Are Coming – How To Be Ready To Track Value-Based Care Outcomes For I/DD Services at the 2023 OPEN MINDS I/DD Executive Summit. Executives Vanessa Yalakidis, Assistant Executive Director of EHR Services of Community Access Unlimited and Julia McConnell, Senior Solutions Consultant, of Qualifacts, discussed how value-based reimbursement models will affect how I/DD service provider organizations track their performance.
Community Access Unlimited is a New Jersey-based nonprofit that serves 3,000 members each year—including people with disabilities and at-risk youth across New Jersey. The programs of the $95,961,803–organization include housing, life skills, employment, personal finance, relationships, civic engagement, and more.
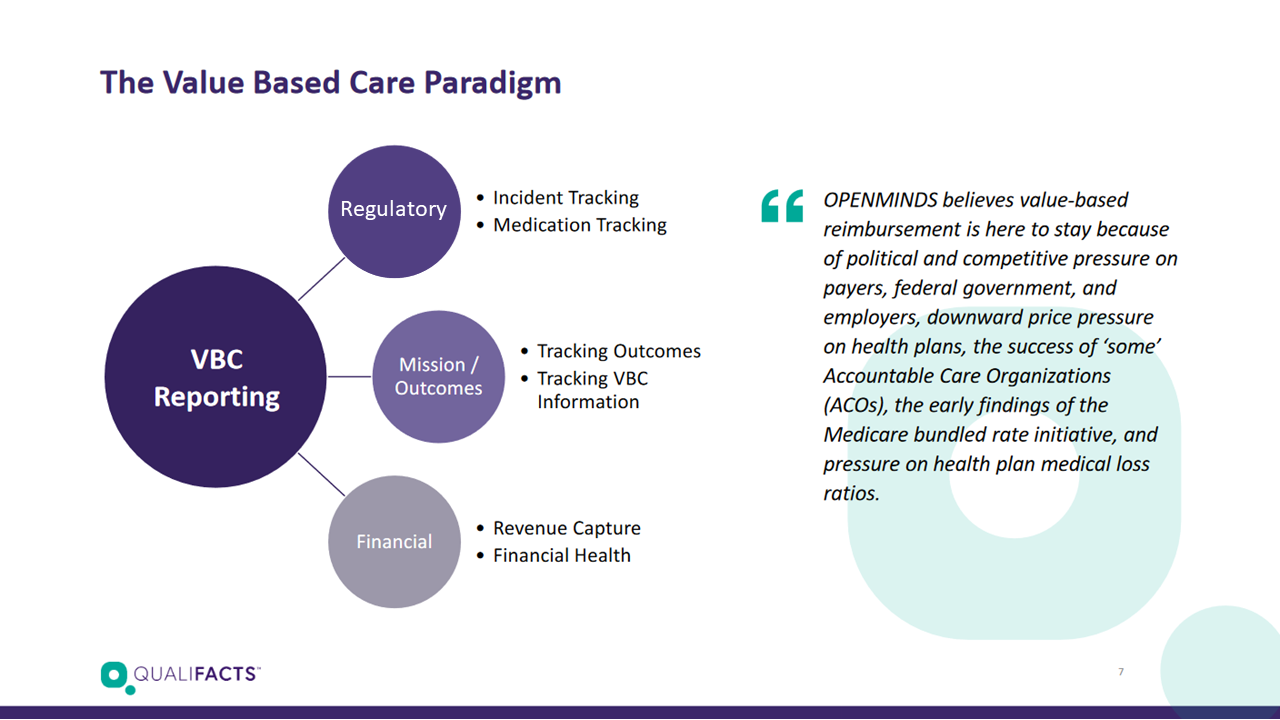
The executives discussed a three-component reporting paradigm for demonstrating and managing quality and value. These three components include regulatory reporting, mission outcomes reporting, and financial performance data.
Regulatory Reporting Almost every contract has some requirements for reporting on performance. This often includes cost data, utilization data, medication reconciliation data, and safety incident data. Executive teams need to plan to gather and report this data as a basic cost of the contract. These are typically measures of import to the customer and often available on to the public. Developing a plan to comply with these contractual reporting requirements in the most cost effective manner possible is critical.
Ms. Yalakidis called for a more elegant solution, “I see where agencies compound the documentation, and they just pile documentation on top of documentation… it’s important to prioritize and streamline for the ease of the systemic modification without impeding your day-to-day operations.”
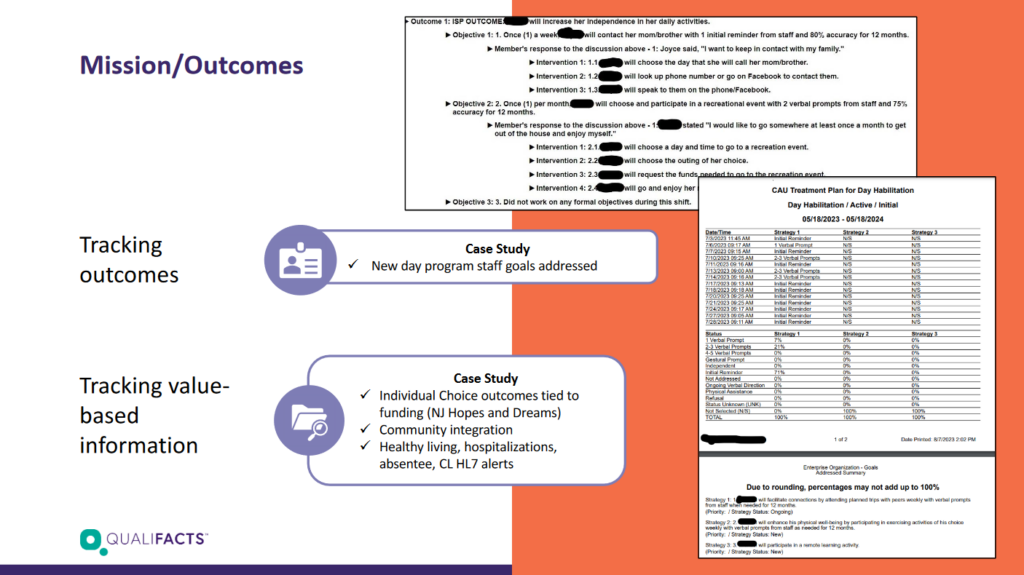
Mission Outcomes Reporting Achieving organizational mission goals is important to a wide range of stakeholders—board and staff members, community stakeholders, donors, and more. Executive teams need to facilitate a process to identify the measures that best demonstrate their contributions to the community and to consumers. This outcome reporting framework often includes demonstrating a focus on the core elements of the “quintuple aim”— consumer experience, population health, cost, clinical experience, and heath equity.
Community Access Unlimited uses an electronic health record (EHR) system to track Medicaid value-based outcomes and ensures they are meeting the individualized support plans of their members. Ms. Yalakidis said, “It’s an opportunity for the managers to review it, making sure we’re doing what we’re saying with each member. The neat thing is staff can see it too. They can see the progress. You can show staff what good work they’re actually doing in their programs.”
Financial Performance Data The move to Medicaid managed often changes the fundamental business model of most organizations. Fee-for-service reimbursement from health plans requires careful monitoring of unit costs, collection rates, cash position, and margins for each service line. And, if there are performance penalties or bonuses—or any type of shared risk—in the reimbursement model, reporting plans need to be adjusted to include those metrics as well.
Ms. Yalakidis talked about using reports to set management priorities, “And I can capture revenue, we batch out Medicaid every week, and my report shows 97% of revenue being captured. When I send that out, not only do I send out what we capture, I send out the reports that show what we haven’t. And that goes to the group managers to show, okay, you’ve got to collect this so that we can get our other 3%”.
As the I/DD service delivery system becomes more competitive and more managed, measuring and managing performance is going to be increasingly important for financial sustainability of provider organizations. Every executive team needs to set their sights on moving their organization—from the board to the front-line teams—to a data-driven perspective. As Ms. Yalakidis said, “Value-based care changes how we have traditionally thought of, and sought, funding for our programs and services. It’s coming and we’re going to have to be able to talk about that as well.”
