By California Health Care Foundation
California’s Medi-Cal delivery system is fragmented. In Medi-Cal, managed care plans are responsible for physical health care and some mental health services, while plans run by county behavioral health departments are responsible for specialty mental health services and most substance use disorder care. When individual Medi-Cal enrollees receive their health care from multiple systems, maintaining coordinated care is a challenge, which can affect their experience and outcomes. To address some of these challenges, managed care plans (MCPs) and behavioral health plans across California are working to create closer connections and better care for their common members. This paper looks at efforts in San Mateo County to streamline operational functions between its managed care plan and behavioral health department with a goal of improving member care and better managing resources.
Health Plan of San Mateo (HPSM) is a County Organized Health System created in 1987 to offer a comprehensive network of providers and to promote preventive care for Medi-Cal enrollees. HPSM currently serves more than 130,000 San Mateo County residents through various health programs and initiatives.
San Mateo County Health (SMC Health) is the county health agency, administering public health programs and providing clinical and supportive services to the community. SMC Health’s Behavioral Health and Recovery Services (BHRS) is the designated county mental health plan for Medi-Cal specialty mental health services and oversees the county’s Drug Medi-Cal Organized Delivery System (DMC-ODS) pilot for substance use disorder treatment services.
SMC Health and HPSM have longstanding collaborations for children’s services, aging and adult services, and coverage, including SMC Health contracting with HPSM to manage the county’s indigent care coverage benefit. HPSM and BHRS also have built effective collaboration and integration efforts related to their respective managed care responsibilities. Since 2007, HPSM has delegated to BHRS all benefits and services for mental health and substance use disorder services for all dually eligible enrollees in HPSM’s CareAdvantage program (also known as Cal MediConnect or Medicare-Medicaid Plan). In addition, from 2014 to 2019, HPSM delegated the Medi-Cal nonspecialty mental health benefit (some- times called “mild-to-moderate”) to BHRS. BHRS has also contracted with HPSM for indigent pharmacy benefits management services and various information sharing functions.
In 2020, HPSM and SMC Health began to define strategies and tactics to achieve improved physical health and behavioral health outcomes for members through greater operational integration.
Objectives
Building on their successful history of collaboration, and their shared pursuit of high-quality member care, SMC Health and HPSM set out to leverage the strengths of each organization across 12 operational functions:
- Call Center
- Care Coordination
- Claims
- Compliance and Oversight
- Credentialing
- Data and Reporting
- Member Rights
- Other Member Services
- Population Health
- Provider Network Management
- Quality Management
- Utilization Management
Both organizations were committed to better supporting existing clinical programs and processes, and to adopting early integration to retain flexibility and control over changes that might be required in the future. Specific objectives were to: A Develop a near-term structure to integrate as allowed under current legal and regulatory
requirements.1 A Identify activities to further integration of health plan and county behavioral health functions under the “Full Integration Plans” proposed under CalAIM (California Advancing and Innovating Medi-Cal) (or a similar structure that might be developed in the future). Under this proposal, the California Department of Health Care Services (DHCS) would support a pilot of Full Integration Plans that integrate physical, behavioral, and oral health under a single entity and contract. The Full Integration Plans would go into effect no earlier than January 2027.2
The Project
Discovery and Request for Proposal Process
The project began with a large internal data collection effort. Through more than 80 data requests and more than 25 informant interviews, HPSM and SMC Health compiled a rich array of background information relative to the 12 functional areas, to support a common understanding of current processes and performance. By assembling this information internally, the project team significantly reduced the cost of the consulting engagement and, equally important, introduced the effort to HPSM and SMC Health stakeholders and gave the core project team a clearer sense of the problems they were looking to solve.
Some of the data that the team looked at are listed in Table 1 on the following page.
HPSM and SMC Health also conducted interviews with over 10 key opinion leaders about integration efforts generally, which helped define requirements for the project and develop a question set for an eventual request for proposals, which was dispatched to 10 potential proposers and received six complete responses.
Consultants from two firms, Mostly Medicaid and Sellers Dorsey, came on board in January 2021 to explore potential integration activities within the 12 administrative functions, prioritize opportunities, and recommend a comprehensive road map for consideration by HPSM and SMC Health. The consultants worked with HPSM and SMC Health leadership and a planning consultant who supported the process.
The process was intensive — consultants and the HPSM and SMC Health team, which included a core of eight senior leaders who were consistently engaged, met at least three times each month. Approximately 40 staff from across HPSM and SMC Health were also involved in the work.


Analysis and Prioritization
Using all the information collected in the discovery phases, the consultant team reviewed policies and procedures, contractual requirements, and state and federal regulations, and interviewed staff from both organizations in each of the functional areas. They presented 85 recommendations for operational integration, which were organized first into tactical categories but then reorganized by the 12 functions.
Some functional reviews, including for call centers and care coordination, led to a deeper analysis of variations in requirements between MCPs and MHPs.
The consultants also offered an approach to prioritization. The core team refined the prioritization approach and used it to review and evaluate the recommendations in a process they described as “pressure-testing” the consultants’ recommendations in discussions of feasibility, impact, and implications. This process greatly improved both organizations’ understanding of the opportunities and challenges.
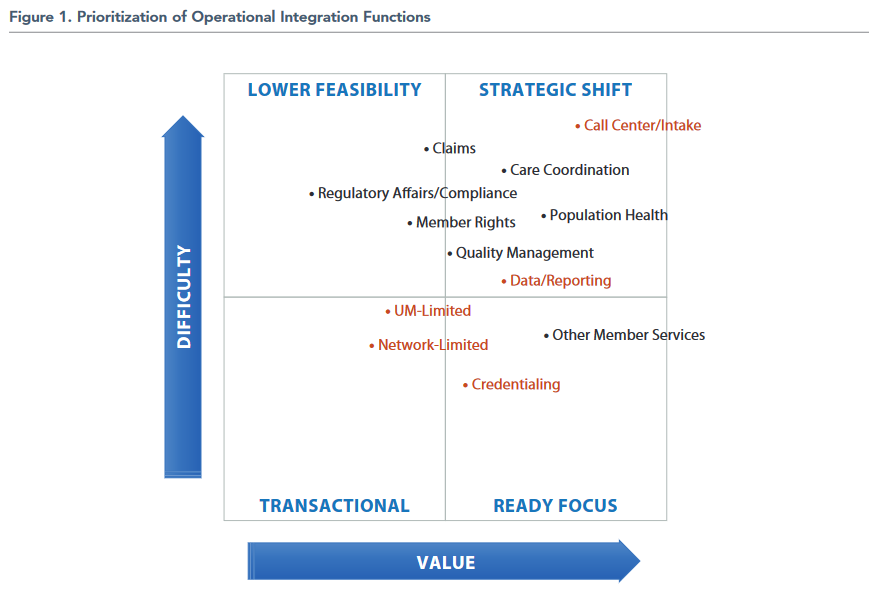
In a final step, the eight core team members ranked operational functions along scales of difficulty/risk and value, and then chose five to prioritize based on (1) their positive impact on member and provider experience, (2) the extent to which they were seen as solving critical program challenges or meeting business needs, (3) organizational readiness, with a goal of finding a balance of more and less resource-intensive efforts. (The five prioritized projects are shown in red in Figure 1.)
Based on this process, the team prioritized the following activities and projects.

Final Decisions
The core team agreed that the most important priority would be the creation of a single call center, both because it was judged to have the greatest positive impact on consumer and provider experience, and because it would not disrupt jobs or raise challenging legal or financing concerns. In addition, the effort would blend existing core competencies for both organizations into a single call center, relying on BHRS staff for their clinical and triage expertise for specialty needs, and on HPSM’s existing strong call center operations and systems, rather than developing new systems. The anticipated benefit would be a single call center leveraging shared technology, providing access to both physical and behavioral health information and resources and creating a more seamless experience for members and providers. The greatest challenge is that the existing BHRS call center is responsible for complying with a variety of specialty behavioral health Medi-Cal requirements as well as triage for local responsibilities such as indigent care and a variety of information and referral calls for non-HPSM members, and these functions must be integrated into HPSM’s systems. This project is expected to start in early 2023 and will require phasing. (Other priority areas may take less time.)
Beyond the prioritization of administrative functions, the consultants helped HPSM and SMC Health create an approach to contracting between the two entities, whereby HPSM would contract with BHRS to provide administrative support in phases. They also created a rubric for the evaluation of future integration activities.
Reflecting on the Project
Challenges
While both HPSM and SMC Health found great value in the process, they also found few “quick wins” in terms of operational integration. Among the challenges:
- Significant variation in program requirements rooted in multiple state and federal agreements
- Different financing systems (MCP and county), which create unnecessary administrative complexity and cost
- Challenges in altering existing provider infrastructure, including information systems
Care management provides a good example of the challenges of operational integration. Across a variety of programs — specialty mental health services, DMC- ODS, HPSM Medi-Cal, HPSM Medicare, and CalAIM Enhanced Care Management (for which regulations were in draft form at the time of this work) — the consultants mapped requirements for these care management activities:
- Assessment: Features
- Assessment: Process
- Care Plan: Features
- Care Plan: Process
- Coordination of Care
- Engagement
- Health Promotion
- Member/Family Support
- Progress Notes
- Reassessment
- Referrals
- Screening
- Transitional Care
- Treatment and Recovery Plan
They found wide variation in requirements, tasks, and frequency across programs, making administrative integration supported by automation highly complex and increasing the risk of program noncompliance were the functions to be combined. They also described the importance of language in the process: The same words mean different things in different systems. Core team members agreed that engaging with questions of administrative integration require this level of mapping, across all functions, in order to understand the opportunities and costs of making these changes.
More generally, HPSM and SMC Health core team members described a fundamental question for plans and counties interested in integrating to any degree: whether to design for the current state of multiple programs and financing sources, or for a future state with more integration among programs at the state level that would in turn reduce barriers to local integration efforts.
Looking Ahead
Some programs within CalAIM could encourage greater cooperation and communication between plans and counties.3 Most immediately, Enhanced Care Management (ECM) requires MCPs to provide care coordination for certain populations. Adults with serious mental illness, substance use disorder, or both are included in the first wave, with ECM required as of January 1, 2022. Under the new Community Supports (CS) benefit, MCPs have the option to offer people with complex needs 14 medically-appropriate services as an alternative to services covered under the Medi-Cal State Plan. These include housing-related services, medical respite, and meals.
In San Mateo, HPSM is contracting with SMC Health for ECM services formerly provided through a Whole Person Care program targeting adults experiencing homelessness and mental health or substance use dis- orders, as well as for ECM and Community Supports for a complex older adult population formerly served through Cal MediConnect. In addition, the changes required by ECM/CS have the potential to push col- laboration between MCPs and counties beyond what is strictly required. For example, as MCPs recognize that their traditional credentialing processes do not work for nonclinical providers of Community Supports, there is an opportunity to align new credentialing processes with those of counties. However, greater operational integration between physical and behavioral health plans is not a central focus of CalAIM, and counties and MCPs that see opportunities to provide better care to consumers through such integration will need to be proactive in making changes.
Other DHCS initiatives, including the Children and Youth Behavioral Health Initiative, the Behavioral Health Infrastructure Continuum Program, and the Home and Community-Based Services spending plan, are designed to improve service capacity, infrastructure, and connection between systems, and could offer additional opportunities for MCP-county col- laboration. HPSM and SMC Health are partnering on the Student Behavioral Health Initiative (part of the Children and Youth Behavioral Health Initiative), for instance.
Lessons Learned
The behavioral health integration planning effort undertaken by HPSM and SMC Health represents just one in a series of cooperative projects between two organizations with a long history of close collaboration. Still, the lessons learned from the project focus as much on culture and communication as on technical planning. As Scott Gilman, director of BHRS for SMC Health said, the process helped the team identify issues and challenges. “Our new mantra is, ‘Let’s talk about it before we build it.’”
Lessons gleaned from the effort include:
- Build from each organization’s strengths and face the challenges.
- Leadership engagement from both organizations throughout is essential.
- Leverage opportunities with key leaders together to discuss broader themes and barriers that may impact more than one area of focus.
- Understand and map the functional requirements from each organization.
- Establish common terms and nomenclature for activities and functional work.
- Interview teams across multiple functions to learn how handoffs and other interactions impact any decisions.
- Have many touch points and opportunities for adjustment throughout the process.
- Prioritize projects with the greatest potential impact and value to consumers and providers, even where they may have more risk or not be the most straightforward.
Even with their long history of working together, both organizations said that the engagement around behavioral health integration with Mostly Medicaid and Sellers Dorsey was unique: “The opportunity to challenge each other, ourselves, and the consultants has allowed for adjustments to be made to make other activities possible in the future.” Both county and MCP participants emphasized that even with regulatory and financial limitations on functional integration, these conversations take time and effort, but “don’t have to be scary” — opportunities to streamline and coordinate processes are available and can improve both provider and consumer experience.
This reprint of “Improving Behavioral Health Systems Through Operational Integration: Efforts in San Mateo County” by California Healthcare Foundation. The original article may be accessed at https://khn.org/news/article/the-boom-in-out-of-state-telehealth-threatens-in-state-providers/.
Reprinted with permission from the California Healthcare Foundation 2022
