Last month, the new behavioral health and social determinants coding changes became effective (see New Behavioral Health & SDoH ICD-10 Coding Changes Became Effective On October 1). Provider organizations must now use the International Classification of Diseases,10th Revision, Clinical Modification (ICD-10-CM) coding, including using Z codes. Those Z codes, for reporting social determinants of health (SDoH), capture factors influencing a consumer’s health status or reasons for utilizing health services.
While many provider organizations have been capturing information about social factors, the Z codes are increasingly important in a health care system that is focused on whole person care models—and reimburses for services that meet health-related social needs (HRSNs). In 2021, CMS released guidance encouraging states to consider social factors in Medicaid managed care and providing more flexibility in covering services that address non-medical needs (see CMS Issues New Roadmap for States to Address the Social Determinants of Health to Improve Outcomes, Lower Costs, Support State Value-Based Care Strategies). As a result, several states have been incorporating SDoH into their Medicaid programs through Section 1115 waivers (see State Waivers List).
The programs to pilot these types of interventions are varied and widespread. Medicaid-funded housing support services are now reimbursed in states like California, Oregon, Arizona, and New York (see Oregon Medicaid Launches Housing Benefits For Individuals Facing Medical Crises and Arizona Medicaid Launches Housing Program For Homeless Beneficiaries With SMI),
North Carolina pays for food-as-medicine programs, among other social supports (see NC Healthy Opportunities Pilot: Food As Medicine Health Care Spotlight). And starting in January of 2025, Michigan will be paying for a number of nutrition-related programs (see Michigan Medicaid To Launch In Lieu Of Services Program To Address Health-Related Nutrition Needs).
Other states have created transportation programs to decrease barriers to attending services while others have programs that focus on identifying and intervening with SDoH issues. For example, New Jersey has introduced Modivcare Medical Transportation program to help individuals access health care appointments (see Modivcare Medical Transportation).

Beyond the states, the Centers for Medicare & Medicaid Services (CMS) is supporting the Accountable Health Communities (AHC) model, a 5-year model that tests whether systematically identifying and addressing the health-related social needs of community-dwelling Medicare and Medicaid beneficiaries has an impact on total health care costs and utilization (see Accountable Health Communities Model). This model requires the collection of standardized SDoH data (see Redesigning Care Around the Social Determinants of Health: A Resource Guide) addressing the gaps between clinical care and community services through screening, referral, and community navigation services.
In addition, the Z codes are becoming more important to health plans and their HEDIS scores. In HEDIS, Z codes can be used to calculate HEDIS measures and identify areas for quality improvement; essentially, Z codes provide a standardized method to report social factors like housing instability, employment issues, or education level on a consumer’s medical record, contributing to a more comprehensive understanding of their health needs beyond just clinical diagnoses (see HEDIS In Action).ed to calculate HEDIS measures and identify areas for quality improvement; essentially, Z codes provide a standardized method to report social factors like housing instability, employment issues, or education level on a consumer’s medical record, contributing to a more comprehensive understanding of their health needs beyond just clinical diagnoses (see HEDIS In Action).
Beyond the states, the Centers for Medicare & Medicaid Services (CMS) is supporting the Accountable Health Communities (AHC) model, a 5-year model that tests whether systematically identifying and addressing the health-related social needs of community-dwelling Medicare and Medicaid beneficiaries has an impact on total health care costs and utilization (see Accountable Health Communities Model). This model requires the collection of standardized SDoH data (see Redesigning Care Around the Social Determinants of Health: A Resource Guide) addressing the gaps between clinical care and community services through screening, referral, and community navigation services.
In addition, the Z codes are becoming more important to health plans and their HEDIS scores. In HEDIS, Z codes can be used to calculate HEDIS measures and identify areas for quality improvement; essentially, Z codes provide a standardized method to report social factors like housing instability, employment issues, or education level on a consumer’s medical record, contributing to a more comprehensive understanding of their health needs beyond just clinical diagnoses (see HEDIS In Action).

Provider organizations can now be reimbursed by some payers for consumer assessment of SDoH and collection of certain Z codes. Medicare Advantage (MA) plans, Medicaid plans, and certain commercial insurers now allow reimbursement for certain SDOH assessments if Z codes are used as part of the documentation. Codes Z55-Z65 address SDoH like inadequate housing, disruption of family, and low income. The HCPCS code G0136 for Assessment Social Determinants of Health (SDoH) has a median national facility rate payment of $8.84, and non-facility rate of $18.66 in 2024 (see Medicare and Medicaid Programs; CY 2024 Payment Policies).
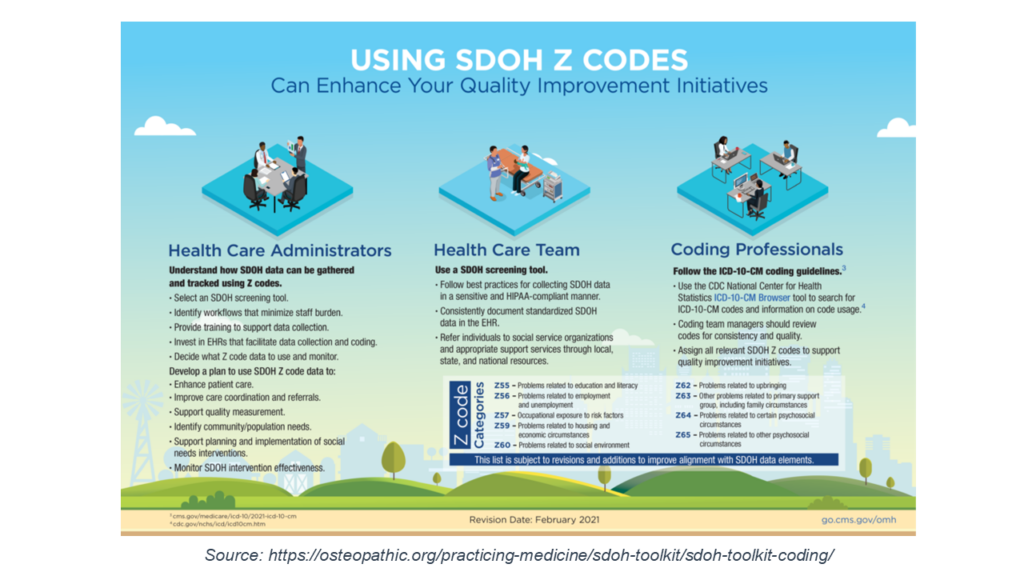
For provider organizations, this shift to collecting Z code data is another requirement that requires both a change in clinical workflow and changes in technology infrastructure. There are many challenges to making this happen. First, provider organizations need a screening tool to standardize collection of the social determinants information. Executive teams need to identify and restructure clinical workflows to accommodate that data collection. EHR systems need to be modified to accept Z-code information. And, there is the need for education of clinical teams on the assessments and the coding (see Z Codes Utilization among Medicare Fee-for-Service (FFS) Beneficiaries in 2017).
As my colleague Sharon Hicks, OPEN MINDS senior associate, advises, these changes mean that provider organizations should be thinking about re-engineering their clinical diagnostic processes right now to ensure that they are assessing SDoH factors and are translating those findings into the correct Z codes. “The only way that payers and managed care providers will be able to use the Z code data is if it is part of the claim form. That means that placing those Z codes in the appropriate field on the claims will be mission critical.”
Developing an organization competency in assessment and coding of social support needs is an important component of participating in whole person care models—and for success in performance-based reimbursement models focused on better consumer health outcomes.
