As Warren Buffet says, “Price is what you pay. Value is what you get.” And the wide differential between what consumers are getting compared to what they’re paying for health care in the U.S. is borne out in the data.
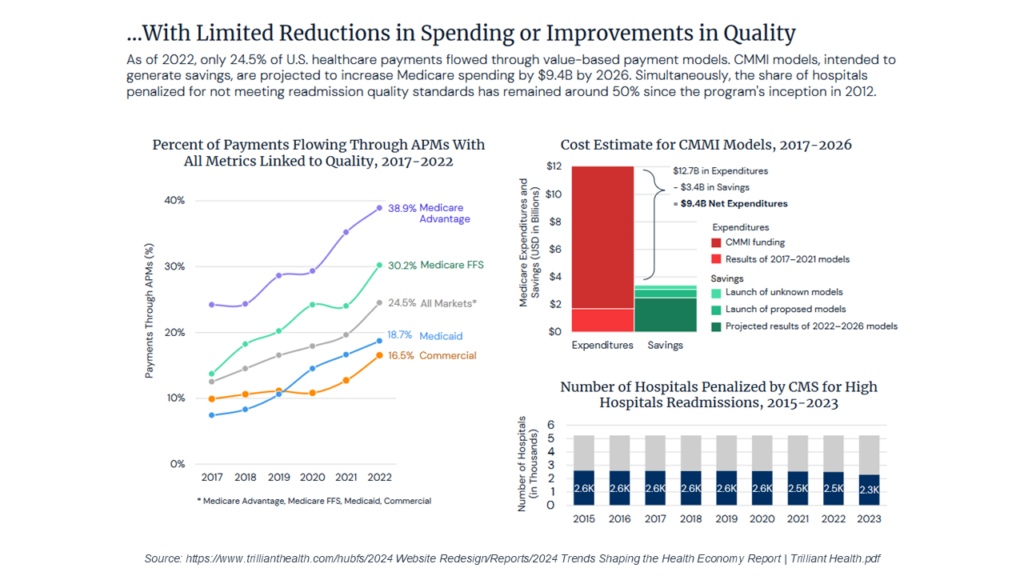
The road to value-based reimbursement has been a choppy one. A new analysis—2024 Trends Shaping The Health Economy—found that as of 2022, 24.5% of U.S. health care payments flowed through some type of value-based payment (VBP) models. This is 17% in commercial health plans, 19% in Medicaid, 30% in Medicare FFS, and almost 39% in Medicare Advantage plans.
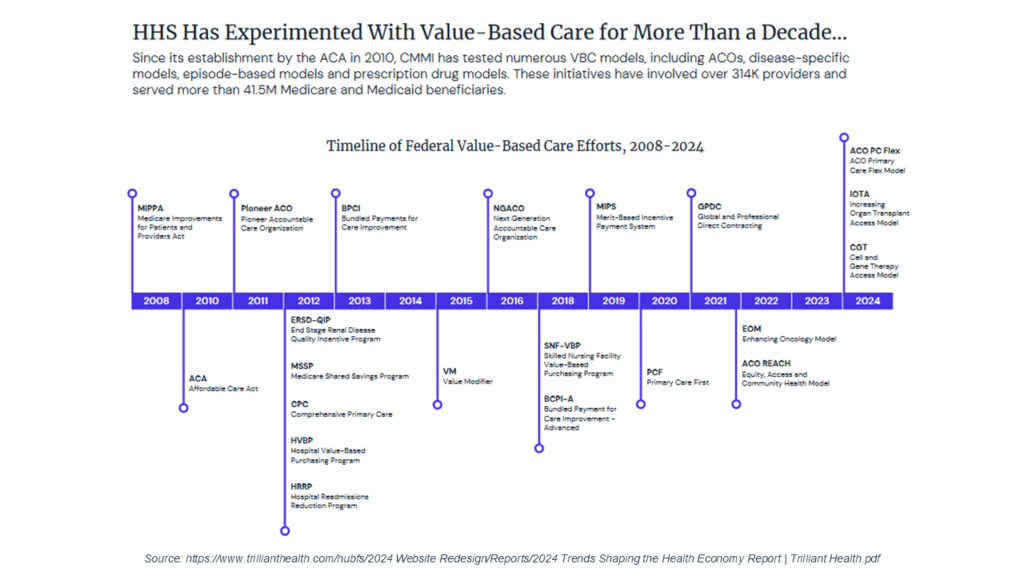
This is due in part to the fact that since 2010, The Center for Medicare and Medicaid Innovation has tested at least 19 different value-based care models, including accountable care organizations (ACO), episode-based models, Primary Care First, MIPS, and bundled payments—with over 314,000 participating clinicians serving 41.5 million Medicare and Medicaid beneficiaries. The effect on bending the cost curve has been minimal (though it was not lost on me that the evaluation of bundled payment methodologies found that only those with provider organizations at full risk produced any savings). The evidence of lack of impact is illustrated in the CMS hospital incentives program. The share of hospitals meeting readmission quality standards has not increased, with the hospitals penalized for not meeting readmission quality standards remaining around 50% since the program’s inception in 2012—little change over a decade.
Despite the fits and starts, we are seeing movement in value-based reimbursement opportunities for specialty care provider organizations. There are Center of Excellence programs with incident-based and longitudinal case rates for acute conditions. There are a growing number of CCHBC programs being paid a prospective payment amount. And health plans are moving to ‘total cost of care’ contracting based on capitation and/or upside/downside risk corridor payments.

The question for provider organization executive teams is how to prepare for a market landscape with 80+ integrated care delivery system models—and just as many approaches to reimbursement. We recently had a chance to hear how one organization is doing that in the executive roundtable, Implementing Value-Based Service Lines: The Mainstay Life Services Case Study, featuring Jodie Esper, Chief Financial Officer (CFO) at Mainstay Life Services. Ms. Esper’s primary advice: CFOs must leverage data to prepare the whole organization, no matter the department, for successful value-based contracting.
Pittsburgh-based Mainstay Life Services is a $26 million non-profit organization that provides residential and support services for consumers with intellectual and developmental disabilities (I/DD), including autism, in Allegheny County, Pennsylvania. Mainstay has one value-based contract for enhanced care management, which began in 2022 with University of Pittsburgh Medical Center (UPMC) Health Plan. The services are reimbursed with a monthly payment amount per beneficiary with quarterly and annual milestone payments. The milestone payments are based on reductions in 7-day and 30-day readmissions, duration and increases in enrollment in the care management program, post-emergency department follow-up, and ensuring competitive employment opportunities for enrollees.
Based on their two years of experience with this new arrangement, Ms. Esper’s advice for other executives as the imperative to create a data driven organization. She said that executives need to know what “data-driven” means; go organization-wide with key performance indicators (KPI); and create a data-driven culture.
Know what “data-driven” means From Ms. Esper’s perspective, being data-driven means three things. First, the data must be transparent throughout the entire organization, from the board to the C-suite and through to the individual program staff. Second, the data must be used to improve the quality of the services the organization. And thirdly, executives need to use the data to make competitive strategic decisions.
“I always tell everybody, please play with the data,” said Ms. Esper. “Look at your data because you cannot break it. It will show you a lot of different information from a lot of different areas, and you can really filter it down to see anything you want. But the most important thing is all the reports and screens may look nice, but if you don’t use it, it has absolutely no value.”
Go organization-wide with key performance indicators Another imperative from Ms. Esper’s experience is the important of having a system of KPI reporting for every business unit and every team. She said that Mainstay combines every data source that it has and delivers weekly reports of all key performance indicators, allowing for faster decisions and faster strategic changes. This organization-wide reporting includes the cost of services (electronic visits, verification, accounts receivable aging), human resources (turnover metrics, recruitment, separation), performance (overtime, productivity, utilization) programs (consumers served, bill units, revenue, productivity, program-specific budget variances, incident management, licensing issues), and quality reporting (health risk screening tools, medical appointments, census, demographics).
Create a data-driven culture To collect and truly leverage the data no matter what the department, Mr. Esper emphasized the importance of executive creating a data-driven culture.
To cement a culture in a place that can take the best advantage of the data and succeed in value-based care, there must be leadership commitment. Mainstay Life Services implemented a series of quarterly operations reviews to bring leadership together. These meetings involve the entire C-suite, department leaders, and program leaders. During the reviews, they assess performance at every level.
“We get people excited and on board,” said Ms. Esper. “That helps us continue to drive and change our organization toward that data-driven culture and a shift to outcomes-driven, value-based care. But change is hard, so I try to hit the staff with the numbers. If you just look at the waiting lists and determine the system of care costs financially, you can see clearly that it’s not sustainable. If we wish to maintain the quality of our services, we must adapt and stay relevant.”
Success in an era of reimbursement based on performance has that single requirement—a data-driven organization—with two key components. The first is having the data—in the right form, at the right time. The second is having a team that knows how to use it—from the leadership team to the frontline employees. VBP has given new meaning to the Peter Drucker adage: “Knowledge has become the key economic resource and the dominant, if not the only, source of competitive advantage.”
