In January, the Centers for Medicare & Medicaid Services (CMS) announced the Innovation in Behavioral Health (IBH) Model, a “No Wrong Door” approach to providing behavioral and physical health services. In June, CMS released the funding opportunity for the model, seeking state applications for the model. Applications were due September 9, selections will be announced in December, and the demonstration is anticipated to run from January 2025 until December 2032.
IBH is a behavioral health-led whole person care model for dually-eligible Medicaid and Medicare members served by community-based behavioral health care provider organizations. The goal of the model is to increase access to services, improve outcomes, and reduce emergency department (ED) and inpatient visits.
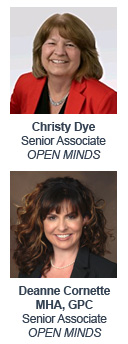
Eligible providers are specialty behavioral health (BH) provider organizations (mental health or substance abuse) who are licensed by the state, enrolled in Medicaid, and provide BH services at the outpatient level of care to adult Medicaid beneficiaries (18 or older) with moderate to severe mental health conditions. The services include screening and assessment for behavioral and physical health conditions, and health-related social needs (HRSN), person-centered planning, treatment and monitoring of behavioral health and physical health conditions, referral and follow-up for HRSNs, and ongoing care coordination.
There are 3 IBH funding sources—up to $7.5M for IT infrastructure, a state-specific Medicaid payment model, and an optional Medicare payment model. And the reimbursement model for those services will be normal and customary billing under Medicare and Medicaid with additional value-based payments for eligible services under the model.
I recently learned more about the model—and how it’s both the same and different than the Certified Community Behavioral Health Centers (CCBHC) model —in the recent OPEN MINDS Executive Roundtable, Doubling Down On Whole Person Care: Advancing Integration Through The CCBHC & IBH Models, featuring OPEN MINDS Senior Associates Deanne Cornette and Christy Dye.
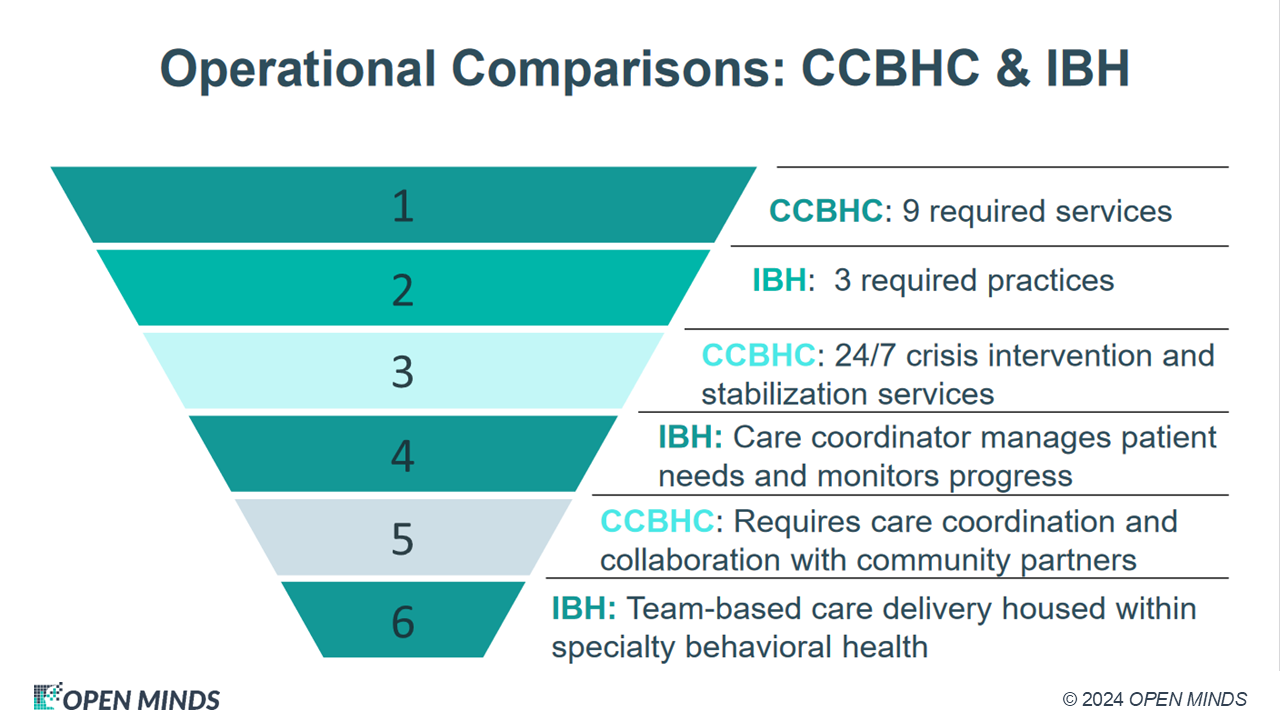
For organizations currently running or considering CCBHC programs, the IBH model offers a slightly different twist. “One of the biggest differentiators is that the IBH model is focused on value-based payment,” said Ms. Dye. “IBH requires a value-based approach in a state’s Medicaid payment methodology—and encourages states to include dual eligibles in their program design for an aligned Medicaid-Medicare approach.”
“A second differentiator is the IBH focus on specific health equity strategies as a required component of the program. And there is the differences in reimbursement. While CCBHCs are paid for nine core behavioral health services, the IBH model does not pay for any services. Instead, it pays for the three enabling processes that support whole person care: care integration (screening, assessment, referral), care management, and health equity. “
Ms. Cornette and Ms. Dye shared a strategic piece of advice for any provider organization considering participating in the IBH model: invest in technology now.
“Whether you are in the planning stage or you already have a whole person care practice, you need a comprehensive technology plan,” said Ms. Dye. “The necessary functionality for success with the IBH model includes integrated electronic health records (EHR), third-party data integration, decision support tools, telehealth, mobile charting, care coordination software, and a population health platform.”
At the center of any technology plan, there must be a fully integrated EHR with interoperability – sharing consumer data with other payer/provider organizations and accepting consumer data from those organizations. The benefits of this interoperability? Provider organizations with interoperability have more expansive data sets and are best positioned to identify high-risk members, know when those consumers have sought outside care (emergency departments, hospitals, public health organizations), create risk scores for those consumers, and identify gaps in care. “You must have the ability to bring in data from external sources and integrate that into your record so that you have a complete picture of the health journey of each consumer,” said Ms. Dye.
Once an organization has the EHR and access to the data needed to make proactive decisions, it also needs the software to facilitate and guide those decisions. This includes a care coordination platform to facilitate the care management process and population health management platforms for proactive care management.
It remains to be seen which of the 80+ integrated care models will become the “standard” in the health and human services field. What we do know is that the higher the level of integration, the higher the financial risk in reimbursement, and the more competency in leveraging technology is the key to success.
