By Monica E. Oss, Chief Executive Officer, OPEN MINDS
The big news on telehealth last week was that the Senate deal to reopen the government will extend Medicare telehealth coverage through January 30. The COVID-era ability of Medicare to pay for virtual care outside of rural health settings expired when the shutdown began on October 1.
Specifically, the extension delayed the reimposition of the geographic restrictions for Medicare non-behavioral telehealth visits and in-person visit requirements for behavioral telehealth visits. The extension also allowed continuation of Federally Qualified Health Centers and Rural Health Centers to remain as distant site provider organizations and reimbursement of audio-only non-behavioral telehealth visits. However, it is unclear if there will be retroactive pay for any virtual care services delivered during the government shutdown.
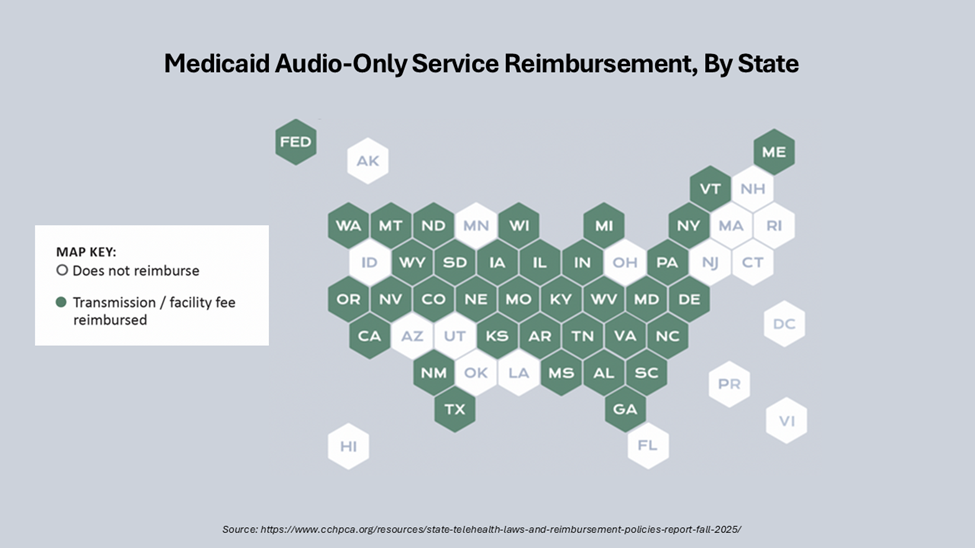
Despite the uncertainty of reimbursement for telehealth in Medicare, the other health care payers have embraced telehealth. According to a recent analysis—State Telehealth Laws And Medicaid Program Policies Fall 2025 and The Center For Connected Health Policy’s (CCHP) Fall 2025 Summary Report—all fifty states, Washington D.C., and Puerto Rico provide reimbursement for some form of live video in Medicaid fee-for-service. In addition, 40 state Medicaid programs reimburse for store-and-forward services; 41 states reimburse for remote patient monitoring (RPM); and 46 states and D.C. Medicaid programs reimburse for audio only telephone in some capacity.
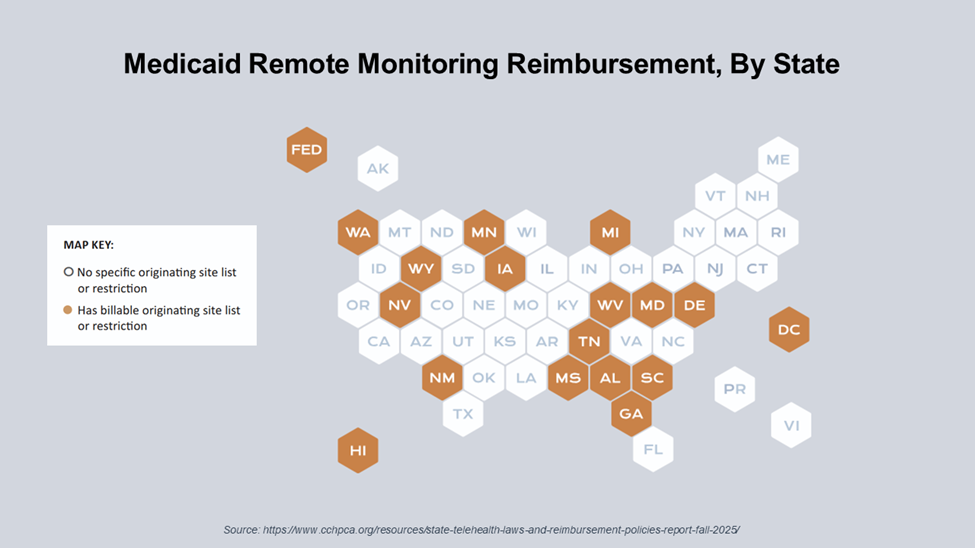
Currently, 32 state Medicaid programs reimburse for all four virtual care modalities—live video, store-and-forward, remote patient monitoring, and audio only. Twenty-four states and Puerto Rico have explicit payment parity for virtual care. Eighteen states, the Virgin Islands, and Puerto Rico have telehealth-specific special registration or licensure processes as an alternative to full licensure for certain types of clinicians.
The study’s authors note that states have continued to expand telehealth reimbursement, including advancing cross state licensing mechanisms through increased participation in interstate compacts and providing targeted licensing exceptions. The question is, what does this evolution mean for strategy and financial sustainability for provider organizations? For answers, I turned to my colleagues, OPEN MINDS Senior Associate Sharon Hicks and OPEN MINDS Executive Vice President Emily Harris.
With regard to strategy, Ms. Harris observed that the expanded virtual care rules and reimbursement create a new scalable operating model for many provider organizations. Her advice is to “assign a clinician licensed in each state to oversee that state’s reimbursement and compliance—then replicate… Think portfolio theory, not silver bullet, matching the licensure pathway to your timeline and risk. The strategy is simple. Use the home for reach and community clinics for economics—don’t build a margin case on fees that are not available.”
She also advised finance leaders to model revenue with realistic state-by-state assumptions. This will require clinical, operational, and reimbursement data to build the workflows, referral processes, turnaround times, and documentation processes that make virtual care easy to use and billable.
Ms. Hicks was equally optimistic about the opportunities in expanded virtual services, but cautioned that there are many administrative challenges. “Services delivered via distributed technology are here to stay, and leaders who have not yet embedded them should use this moment to close the gap. The opportunity is real. But, so is the audit trail.”
“The worst outcome,” Ms. Hicks warns, “is getting paid and later facing takebacks for non—compliant claims. Multiple Medicaid programs have retired 99441 – 99443 in favor of standard evaluation and management (E/M codes) with modifiers, some have adopted new American Medical Association telehealth codes, and others publish telehealth-specific lists or communication technology-based services pathway references that matter at the claim line level.”
Ms. Hicks advises management teams to consider two adjustments. “First, align billed codes with the treatment actually delivered, and make sure documentation captures any escalation of acuity during the visit. Pair that with a lightweight onsite audit function empowered to adjust claims when the record supports higher acuity, and with clear rules for when audio-only is appropriate versus when video or in—person and clear rules for when audio-only is appropriate versus when video or in-person is required. The policy trajectory is embedding these expectations in black and white… Lead with the encounter code, let PPS do its job, and stop chasing ancillary payments that will be denied.”
To make this happen at the service level, she noted that “Revenue follows workflow, without a clean referral and documentation loop, there is no sustainable line of business… Inventory your highest volume visits, quantify reimbursement by code and modality in each state, and either swap to alternate codes or realign offerings to what is actually reimbursable… Pick the fewest high yield moves and execute relentlessly—go wide later.”
Telehealth is now infrastructure, and the winners will be the operators who execute with precision—standardizing consent, engineering claims to state rules, building hub-and-spoke site economics, and scaling only what performs. Ms. Harris observed that the path from policy to P&L is disciplined, not flashy. “Make the payment model your ally—align telehealth documentation and modifiers to the value-based rules you’re actually paid under.”
