By Monica E. Oss, Chief Executive Officer, OPEN MINDS
The bad news for employers, federal and state payers, and health plans is that the medical cost trend for the year ahead is at 8.5% for the second year in a row. The new analysis, Medical Cost Trend: Behind The Numbers, identified three key drivers—pharmaceuticals, hospital costs, and behavioral health spending.
The pharmacy cost trend is actually 2.5 points higher than the medical trend, with a $50 billion increase in pharmacy spending in 2024 (up from a $20 billion increase in 2023). The analysis attributes this increase to expanding use of GLP-1s and new drug launches.
Another reason for the trend is increased hospital spending. Hospitals are both increasing rates and increasing the yield on their billing through enhanced revenue cycle management (RCM) practices. For hospitals, the driver is inflation. Wages are rising more quickly for employees of hospitals than the national average. Tariffs are also contributing to that inflation—and that effect will be more pronounced in the rest of this year. The result of this inflation is reflected in their margins. In 2024, hospital year-end margins were, on average, 2.1%, compared with 7.0% in 2019.
Utilization of inpatient and outpatient behavioral health services is the third factor contributing to the rising medical trend, with a 45% increase in behavioral health claims between January 2023 and December 2024. Claims for inpatient behavioral health services were up nearly 80% between January 2023 and December 2024. For outpatient services, claims were up nearly 40% over that same period. And health plan actuaries expect a 10% to 20% trend for behavioral health expenditures in the year ahead.
The authors of the analysis conclude, “Rising costs are a driving force making health care transformation inevitable.” Specifically regarding the rise in behavioral health costs, they recommend that health plans move to condition-based alternative payment models, including capitation models.

These cost pressures raise fundamental questions for health and human service executives—what does that health care transformation look like? And what are the models that will work in moving away from paying for volume, to paying for value? We got a behind-the-scenes look at how one organization moved to up their performance in the OPEN MINDS Executive Roundtable, Building A Quality & Safety Infrastructure: The Harris Center Case Study, featuring Luming Li, M.D., Chief Medical Officer, and Trudy Leidich, Vice President, Clinical Transformation and Quality at The Harris Center for Mental Health and IDD (the Harris Center). They shared their journey to improving organizational performance and reliability.
The Harris Center is the mental health and intellectual and developmental disability (I/DD) authority for Harris County, Texas. With a budget of $375 million, it serves 90,000 consumers each year and responds to approximately 130,000 crisis calls.
The Harris Center’s value improvement initiative has focused on becoming a “Highly Reliability Organization” (or HRO)—an organization with standardization of processes and a prioritization of quality and safety.
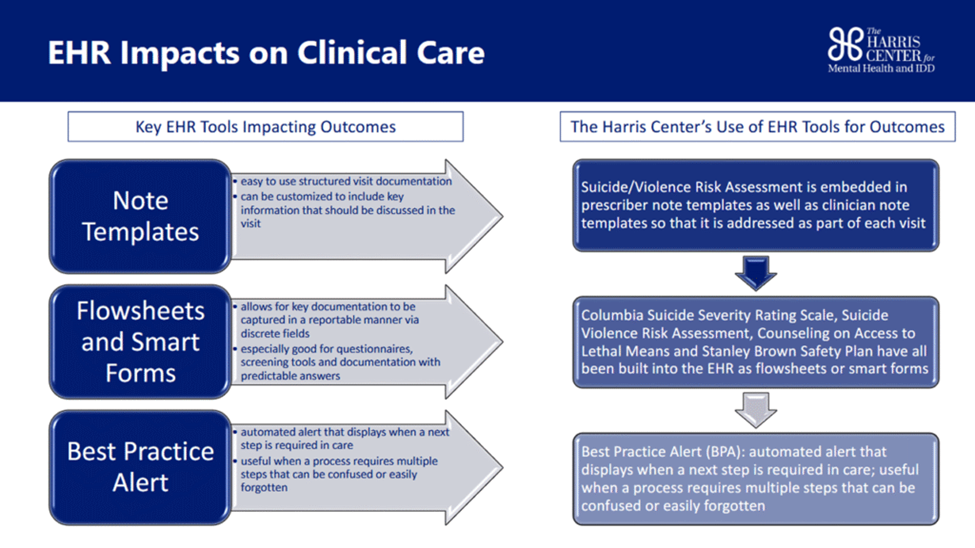
To achieve this transformation, the Harris Center developed a formal performance improvement plan; enhanced its performance reporting; and increased its formal review of critical incidents and performance data. This included a central data warehouse that integrates event reporting, clinical outcomes, and analytics, and a software tool to track critical incidents.
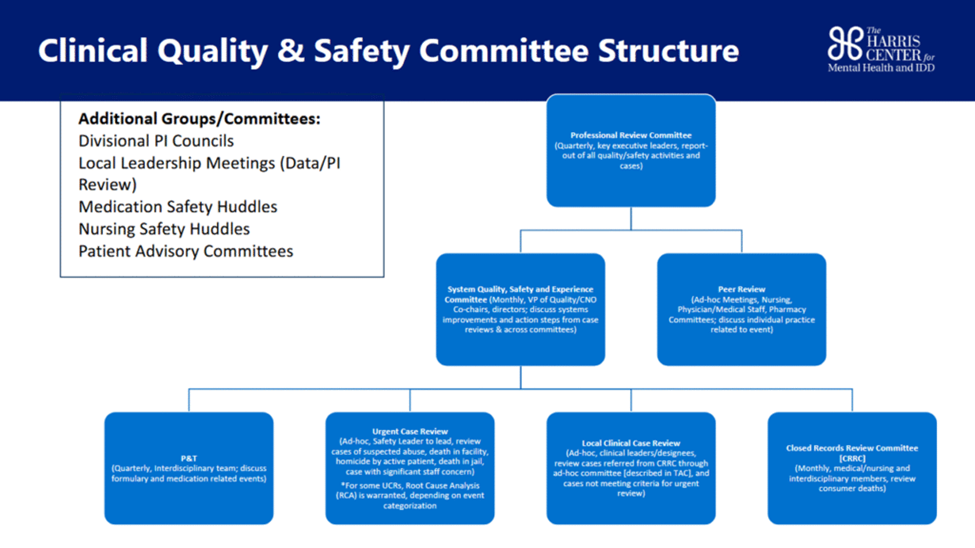
To support this transition, the Harris Center also restructured its leadership team and created six clinical review committees as well as a System Quality, Safety, and Experience Committee. And to increase understanding of the new model, an enhanced staff and leadership training program was launched.
The results of their HRO initiative have been striking. Over 93% of consumers now have a same-day risk assessment, and there is same-day safety planning for 87% of consumers.
For executive teams who are looking to enhance their delivery system performance, Dr. Li and Ms. Leidich offered three pieces of advice. First, executives need to design their systems to define performance and critical incidents—and measure them. Second, performance data should be the driver of management decisions. Thirdly, training is critical to making performance improvement plans a reality.
At the outset, executives need to define the performance they want—and the incidents they want to avoid—as part of planning performance improvement. This means making those measurements a standardized and repeatable part of daily operations. Ms. Leidich said that the organization uses both the root cause analysis (RCA) framework and the failure mode and effects analysis (FMEA) process to identify when the system was causing errors to operationalize improvements.
“It’s very easy to say, ‘This is the outcome that happened, and this is what we want to do to fix it,’” said Ms. Leidich. “But we know that events happen because system and process issues usually exist. We help people do the right things by putting it into our processes.”
Next is creating a culture and standard operating practices to act on that data. This means integrating data from as many sources as possible. The Harris Center relies on event reporting and service-level data to track performance, safety, quality, and outcomes for all programs and populations—and then commits to full transparency by sharing that data across departments.
“If you’re not transparent with outcomes, you won’t improve,” said Ms. Leidich. “We needed a mindset that learns from mistakes and uses data to drive decisions.”
To build a high-performing organization, executives need to gain access to a diverse array of strengths and skillsets to build on existing success and then commit to the complex and evolving demands of system-wide improvement. The Harris Center purposely built an interdisciplinary quality department with intentionally varied backgrounds—from Lean Six Sigma experts to clinical nurses and data scientists.
Finally, performance improvement requires new operational skills—which can be acquired either by upskilling existing team members or with new hires. When the system data identifies errors, they need to be addressed with daily safety huddles and performance improvement councils. “We had to hire the right people and give them the freedom to do the work,” said Ms. Leidich.
“Part of the learning for us is developing a structured tool and a structured set of workflows to guide the clinical team,” said Dr. Li. “In addition, there’s the human side of it, which is mobilizing teams to move away from what they were doing before, to then ease and support them into doing their work in a different way.”
