By Monica E. Oss, Chief Executive Officer, OPEN MINDS
The focus on health outcomes is stable but shifting. The data in a new survey report—Optimizing Health Outcomes For All—surveyed key opinion leaders across the health and human service system and found that most (86%) expect their organization’s prioritization of health outcomes to remain consistent or increase even amid the evolving external landscape.
However, nearly two-thirds (62%) of executives reported plans for reducing investment in at least one health outcomes area. What is growing are initiatives focused on health care access (56%) and affordability (34%). The survey also found there is a declining emphasis on non-medical social determinants of health. Currently, 67% of provider organizations are collecting data on social determinants of health, and 58% on clinical outcomes by subpopulation. This compares to 74% and 52%, respectively, for payers.
Most public sector health care executives anticipate an increase in prioritization of health outcomes activities (75%). They emphasize the larger role that community connectivity and societal impact play in driving their health outcomes agendas. But the survey authors noted that the defunding of federal programs may jeopardize their ability to translate this prioritization into tangible impact. In contrast, provider organization executives report the greatest anticipated decrease (27%) in health outcomes initiatives due to the external environment.
The report authors noted that respondents reported that outcomes initiatives are key to securing and succeeding with value-based reimbursement (VBR). Looking ahead, 58% of executives expect minor federal policy changes in health care, while 31% expect major changes. While expectations on scale and impact are mixed, there is clear agreement that the health policy landscape will remain dynamic.
We had an opportunity to learn more about how one organization—The Columbus Organization (Columbus)—is using health outcomes data to drive person-centered care in the session, Developing A Person-Centered Approach To Care Delivery For Aging & Medically Complex Populations: The Columbus Organization Case Study at The 2024 OPEN MINDS Technology & Analytics Institute. Tanya Wyant, Ph.D., Vice President, Northeast–Care Coordination, and Elaine Aguirre, M.D., Vice President of Clinical Operations for Columbus, provided perspectives on using data to support a whole person care model.
Columbus is a for-profit provider organization in Pennsylvania that provides health care services in nine states and employs 500 people. It provides integrated care and care coordination services for consumers with complex health needs, including individuals with intellectual and developmental disabilities (I/DD) and aging consumers. Columbus reaches nearly 17,000 consumers each year.
The evolution of Columbus’ approach started with the challenge of serving individuals with I/DD who are living longer. As a result, existing Medicaid home and community-based services and waiver services often don’t address their needs.
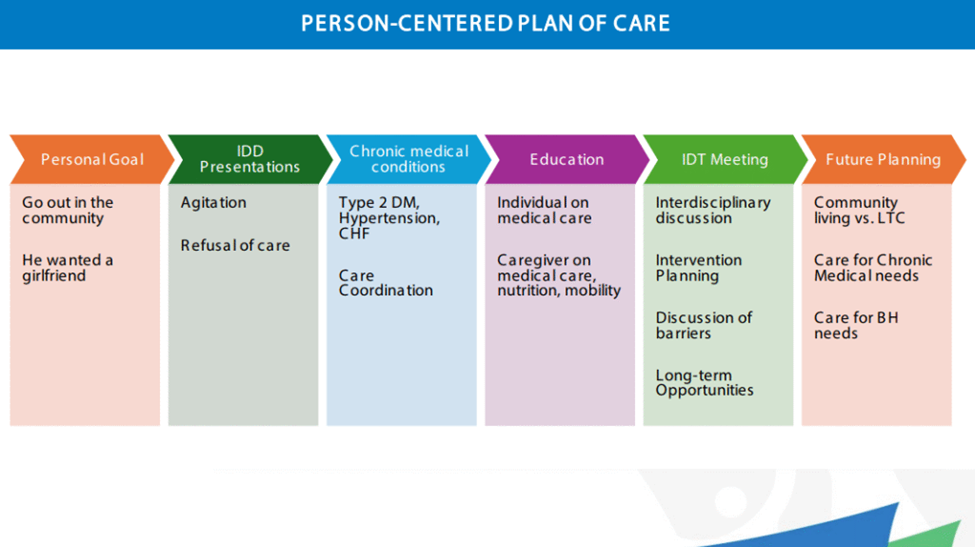
To address this issue, Columbus shifted from a traditional case management model to a multidisciplinary care management model that uses data to drive complex care management with a whole person care model. The model is driven by an individualized person-centered care plan that is adjusted monthly to reflect medical and social needs, as well as personal goals and aspirations of the consumer. To support the model, Columbus adopted a proprietary dashboard for data-informed care management to track individual outcomes and population-level trends.
Dr. Wyant and Dr. Aguirre offered some insights to other provider organization executives who are considering using data to improve their approaches to whole person care—and VBR contracts for those models. The first is to design data systems to anticipate individual consumer needs while positioning the organization for long-term sustainability. The other is to plan the model for use with future VBR arrangements.
The care management data driving whole person care has two simultaneous uses. The first is to have relatively real time data for each consumer that supports proactive care management—allowing staff to identify risks earlier and guide decision-making. This includes connecting social interventions (housing, transportation, socialization) with consumers’ clinical outcomes. The second is to provide the collective information to position the organization as a population health manager by identifying trends across the consumers served.
“We really looked at the data to harness the individual’s life, to see, wow, they’ve had multiple hospitalizations and readmissions and were homeless six times out of the year,” said Dr. Wyant. “We can look at this data and ask how we can fix it. How can we manage this better over time by getting the right care team involved, not only as a choice for the individual but also to help them as they transition through life?”
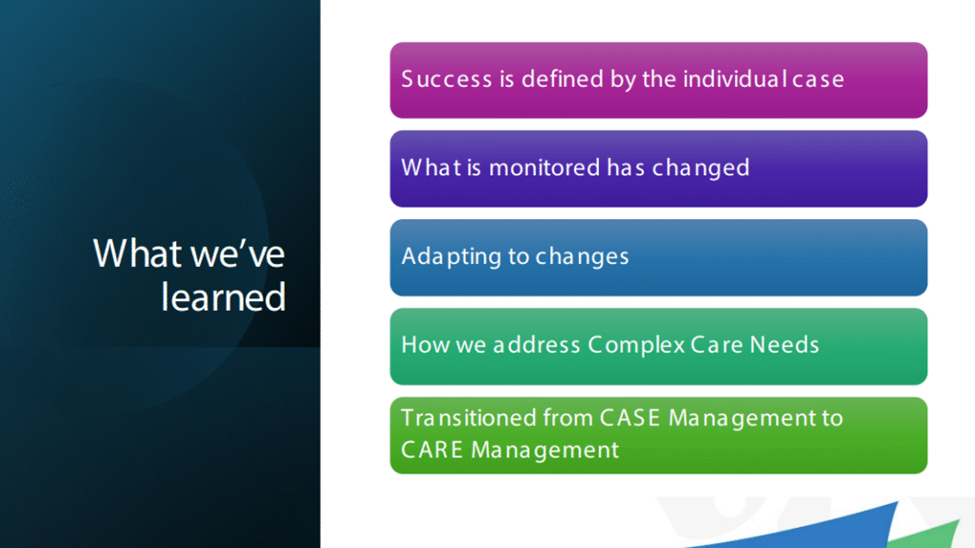
Related to that population health management competency is the (related) ability to manage VBR arrangements. This includes the ability to measure the performance data of most interest to payers—like total cost of care, care access times, readmission rates, and follow-up after hospitalization.
As the health and human service system adjusts to the many recent federal policy changes, the use of whole person care models in integrated delivery systems is likely to increase. As Dr. Aguirre noted, “How we address the complex needs for individuals can vary, and it’s not one size fits all. We have to adapt to change.”
