By Monica E. Oss, Chief Executive Officer, OPEN MINDS
The cost of Medicaid services has the attention of state legislatures. Colorado is assessing their options. The Colorado Medicaid Provider Rate Review Advisory Committee is recommending a plan that is different, and more expensive, than the proposal from the governor’s office.
In California, the Legislature’s Nonpartisan Fiscal And Policy Advisor just released their Medi-Cal budget report—Medi‑Cal Fiscal Outlook. It points out the largest driver of growth ($12.8 billion) comes from Increases in member utilization and rate increases. And Utah’s economists are concerned about paying for Medicaid in 2026. The federal government funded 64.4% of Utah’s Medicaid program in 2025, but the economists are making future projections for a future in which the federal government covers 50% of the program.
Medicaid per-member spending varies widely across states. Medicaid spending ranged from $4,780 to $12,295 per member in 2023, with national median spending per member at $7,909. States such as Alabama, Florida, Georgia, and Nevada have some of the lowest spending, while Washington, D.C., Minnesota, Pennsylvania, and North Dakota report the highest spending. About one in seven states spend more than $10,000 per member Spending also varies widely by Medicaid eligibility group. National average per member spending is $20,950 for people with disabilities, $20,194 for senior members, and $3,321 for children. Per member spending for people with disabilities shows the greatest variation, from $5,040 in Florida to $57,900 in Minnesota. In contrast, children’s per enrollee spending ranges less from $2,227 in Alabama to $5,457 in Alaska.

Not surprisingly, states have (and will likely continue to) adopt different strategies to increase value and reduce costs. Our recent analysis—Medicaid Care Coordination Initiatives: A State-By-State Guide—found all states have adopted some type of Medicaid care coordination initiative. There are currently 199 different initiatives up and running.
The states with the most adoptions of Medicaid care coordination initiatives are Idaho, Iowa, Massachusetts, Minnesota, New York and Rhode Island. And over the past five years, the states with the greatest increase in the number of care coordination initiatives include California, Idaho, Illinois, Iowa, Minnesota, and Rhode Island. In contrast, the states with the fewest adoptions of care coordination initiatives are Alaska, Georgia, Indiana, Kentucky, Louisiana, Montana, Nevada, New Hampshire, South Dakota, and Wyoming. Oklahoma was the only state that reduced the total number of Medicaid care coordination initiatives adopted.
The greatest change between 2019 and 2024 was the number of states with certified community behavioral health clinic (CCBHC) initiatives—20 states in 2019 and 48 states by 2024. The largest decrease was in the use of ACA model health homes—30 states in 2019 and 21 states by 2024. There was no change between 2019 and 2024 in the number of states with Medicaid managed care.
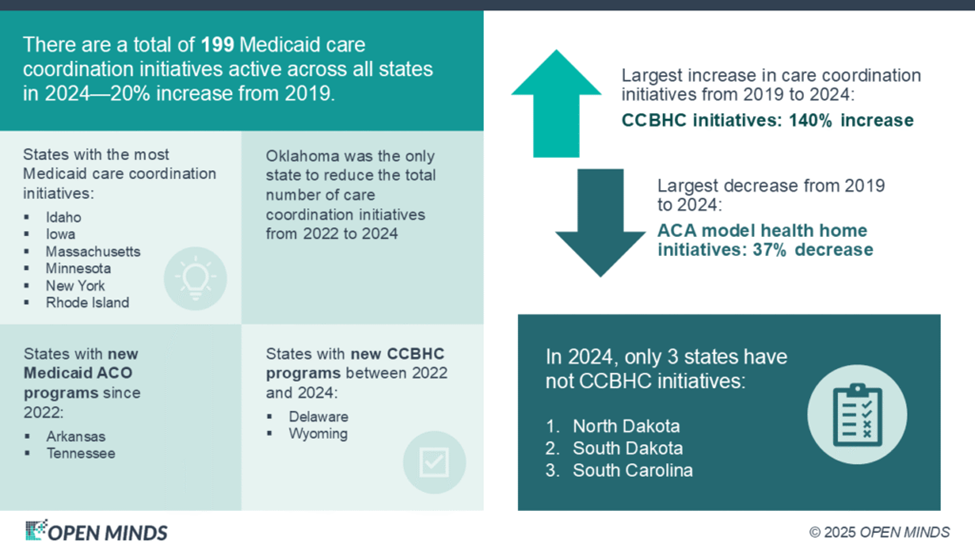
There are now 47 states, plus the District of Columbia, that have an active CCBHC initiative. The most recent additions to this list are Delaware and Wyoming. Only North Dakota, South Carolina, and South Dakota have not adopted some type of CCBHC initiative.
