By Monica E. Oss, Chief Executive Officer, OPEN MINDS
“Can we do better than the airlines?” That was the provocative question asked by Matthew O. Hurford, M.D., Chief Executive Officer of Community Care Behavioral Health (CCBH) and Vice President of Behavioral Health at University of Pittsburgh Medical Center (UPMC) Insurance Services, at the 2025 OPEN MINDS Executive Leadership Retreat, during his session, Collective Impact In Behavioral Health: Lessons From The Airline Industry.
Given the data, the answer is “not yet.” The U.S. spends more per capita on health care than any other country—at 17.6% of GDP in 2023. But the U.S. also has poorer outcomes in areas like maternal health and post-operative complications. And the costs will likely continue to increase. Analysts are projecting an 8.5% increase in group health insurance costs and a 7.5% increase in individual health policy cost in 2026, according to a new analysis, Medical Cost Trend: Behind The Numbers 2026.
Behavioral health treatment costs are near the top of the list in terms of drivers of that medical cost inflation. Utilization of behavioral health services rose 44.6% from January 2023 to December 2024, with a nearly 80% rise in behavioral health claims for inpatient services between January 2023 and December 2024. And utilization is trending upwards across most conditions—with developmental, anxiety, and depressive disorders seeing the largest increases.
The analysts note that these behavioral health utilization trends are driven by the system’s siloed structure—disconnected care pathways, misaligned financial incentives, and poor data exchange. As a result, there will be continued pressure on health plans to develop condition-based alternative payment models, such as a capitation model or collaborative care models.
These findings illustrate the contention of Dr. Hurford that the behavioral health treatment system is not operating like an optimally coordinated system. Hence his airline comparison. Dr. Hurford’s belief is that the health care field needs to adopt the Collective Impact Model found in the airline industry—which he described as a collaborative framework with five core principles: a common agenda, shared measurement, mutually reinforcing activities, continuous communication, and backbone support.
“In a year, there are approximately 36 million flights carrying 5 billion passengers with a customer satisfaction rate of 74%,” said Dr. Hurford. But in the behavioral health sector, “40 to 50 million people in the U.S. received treatment in 2024, yet the consumer satisfaction rate is only 66%.”
In the airline industry, a common agenda for consumers and businesses includes arriving in comfort, timeliness, profitability, and safety. Shared measurements include on-time performance and customer benefits like frequent flyer programs and airport lounges. Interconnected communication facilitates interoperable scheduling systems. Not surprisingly, these standardized and shared measures are not found to the same extent in the health and human service field.
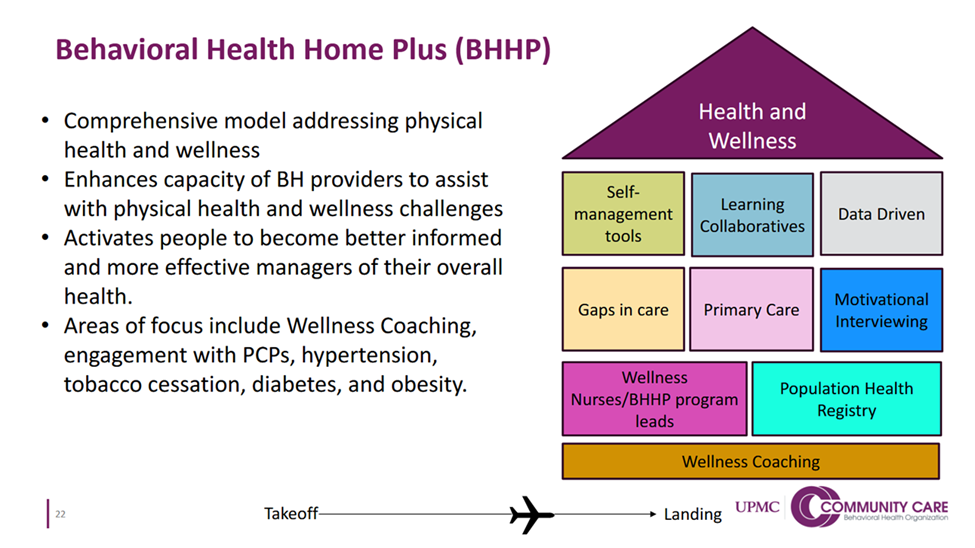
Dr. Hurford highlighted several models illustrating how CCBH, as part of UPMC Health Plans, is applying the Collective Impact Model to behavioral health care. One example is UPMC’s Behavioral Health Homes Plus (BHHP) program, a comprehensive, patient-centered model that integrates physical health and wellness into behavioral health services for adults with serious mental illness and other complex conditions. The model extends provider organization capacity through wellness coaching and interventions for hypertension, tobacco cessation, diabetes, and obesity—using self-management resources, motivational interviewing, data-driven population health registries, and wellness nurses.
The participating behavioral health provider organizations acting as health homes receive capitation payments from CCBH to provide services. Those payments are tied to quality metrics and outcomes. Dr. Hurford noted that this value-based approach rewards reductions in care gaps and wellness improvements through enhanced payments for coaching, coordination, and preventive care.
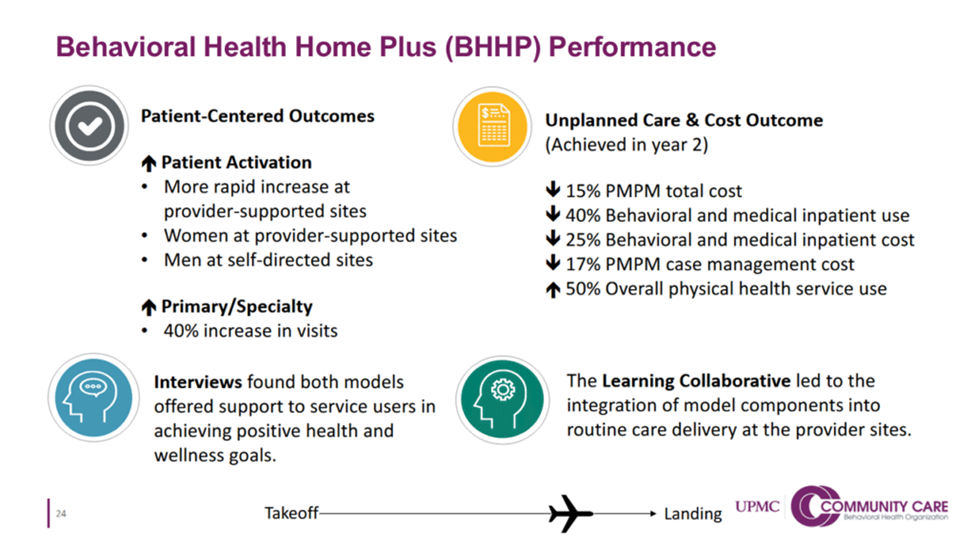
The BHHP program has accelerated consumer activation—with 40% increases in primary and specialty care visits. In the second year, the model reduced total per member per month (PMPM) costs by 15%. This was due to a 40% reduced inpatient utilization, a 25% inpatient cost savings, and a 17% case management savings.
Dr. Hurford had some advice for other health plan/provider partnerships—forge a common agenda and while thinking big, start small with launching and testing pilot programs. In the spirit of the Collective Impact Model, the first step is aligning partners on shared goals like recovery, quality, timeliness, margin, and safety.
In making that common agenda a reality, his advice is to think big about what a partnership is trying to achieve—with common accountability and success metrics. But the key on the path to that big vision is to start small—and create pilots to test the model and the relationships.
Dr. Hurford closed with his thoughts on how collaboration can improve health care as it has the airlines industry. “No one industry has figured out the secret sauce…the urgency of what’s before us is larger than what our system can manage alone.”
